Lesson 2: The Wildcard, Part I: How SARS-Co-v2 Can Disrupt Your Immune System
Lesson 2 Protocol 1
To learn enough about a SARS-CoV-2 infection and the potentially health-compromising COVID-19 illness that you are motivated to do Protocols 2, 3 and 4.
The five basic things to remember about SARS-CoV-2:
- This virus is a respiratory virus that infects you via the mouth, nose and eyes.
- It can spread undetected by your immune system for two days or longer, thereby spreading its infection to various tissues in the upper and lower respiratory systems and beyond.
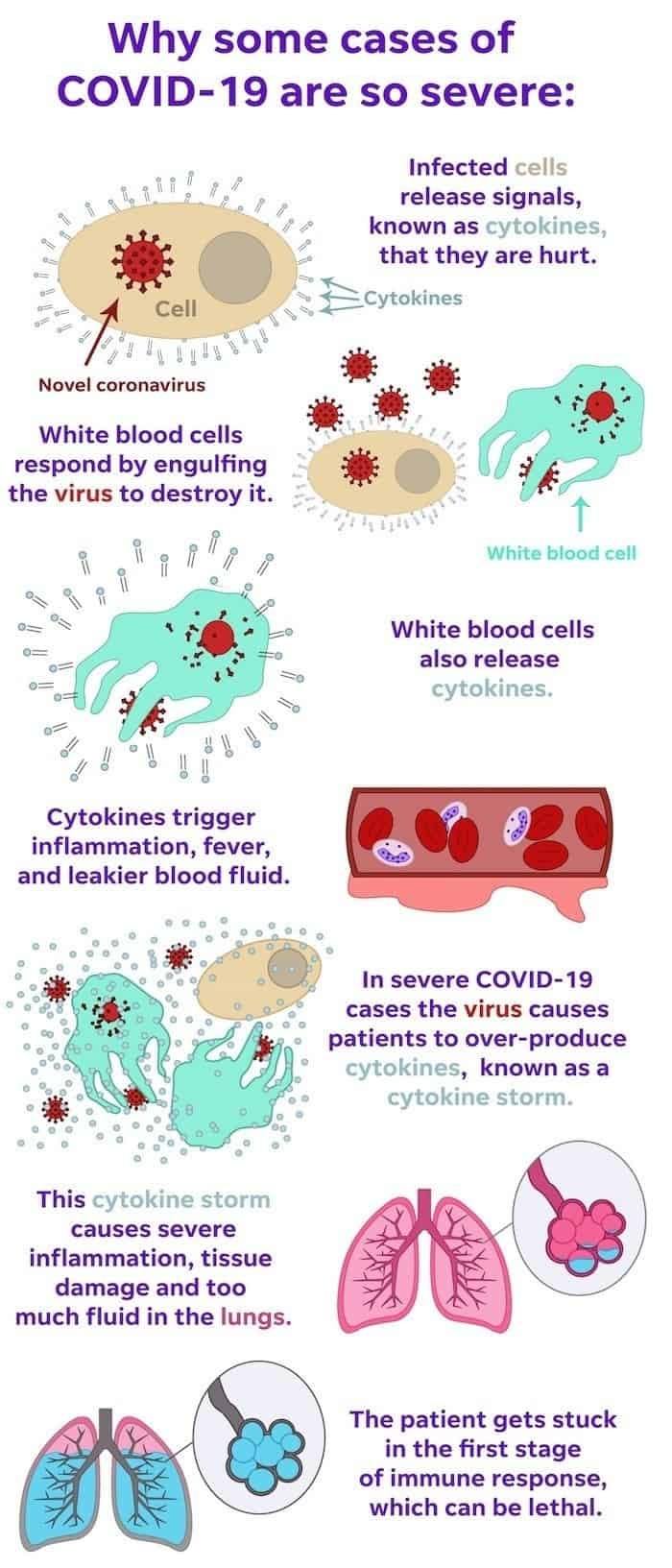
- It can produce excess inflammation that can cause a dangerous hyperinflammatory condition called the “cytokine storm”.
- Some people can get infected and be asymptomatic, having no to few minor symptoms; whereas others can get deathly ill.
- The most vulnerable are the elderly and those with chronic illnesses. (See Lesson 10.)
The Wildcard, Part I: How SARS-CoV-2 Can Disrupt Your Immune System
Any virus that can make people sick has at least one good trick for evading the immune system. For SARS-CoV-2 that trick is stealth.
Because it’s stealthy, it can evade recognition and thereby delay the launch of the innate immune system, and inhibit the production of interferons—those molecules that initially block, or “interfere” with viral replication.
This delay creates a brief time window in which the virus can replicate unnoticed before the immune system recognizes it as a foreign pathogen alarm and kicks into action. This is why it can take two or more days for symptoms to appear after infection.
Those delays can cascade; meaning, if the innate branch of the immune system is slow to mobilize, the adaptive branch will also lag. (This will be addressed in greater detail in Lesson 12 when discussing the “domino effect”.) What then can wind up happening is that the immune response is caught in a continuous loop of activation and inhibition.
The result of this immune system cascade is that the normal, initial inflammatory phase is overstimulated. This is dangerous if it leads to hyperinflammation because it can damage critical organs. The lungs, the heart and other organs can't withstand a severe inflammatory response for too long.
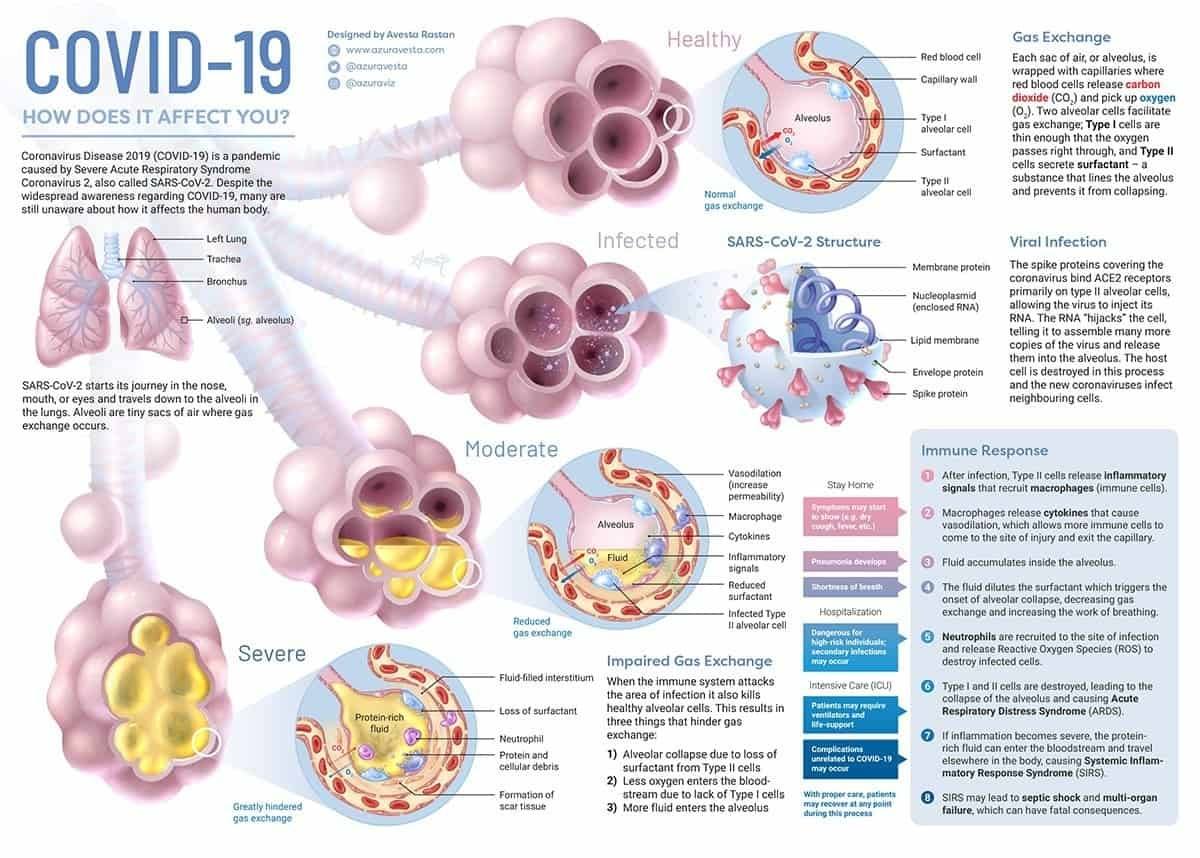
For the lungs in particular, leakier blood can flood the air sacs with fluid, making it harder for you to breathe and get oxygen needed to keep other organs functioning.
SARS-CoV-2 Infects The Respiratory Tract
As the name reveals, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is a respiratory infection, and it makes the lungs vulnerable to COVID-19, the disease caused by the SARS-CoV-2, because it presents as a lower-respiratory tract infection, similar to bronchitis and some strains of the flu.
Lower respiratory tract infections differ from the more common upper respiratory tract infections:
- Upper respiratory tract infections, which include most strains of the common cold, tonsillitis, and sinus infections, are primarily characterized by symptoms above the collar--runny nose, headache, sore throats.
- Lower respiratory tract infections take root below the larynx and therefore are more commonly associated with coughing, fatigue, and shortness of breath.
In a viral lower respiratory tract infection, the virus enters the body through the nose, mouth, or eyes, and travels down the respiratory tract in search of a host cell. Viruses cannot reproduce on their own and therefore need a host to “hijack,” overriding the cell’s normal function with a new command:
Reproduce the virus.
Once the virus fills up the cell, the cell will burst, and the newly formed virus will then set out in search of even more host cells.
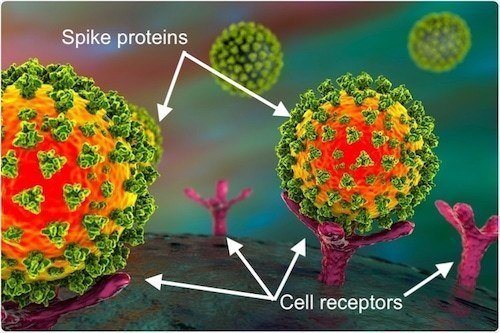
Like other coronaviruses, SARS-CoV-2 particles are spherical and have proteins called spikes protruding from their surface. These spikes latch onto human cells, then undergo a structural change that allows the viral membrane to fuse with the cell membrane. The viral genes can then enter the host cell to be copied, producing more viruses.
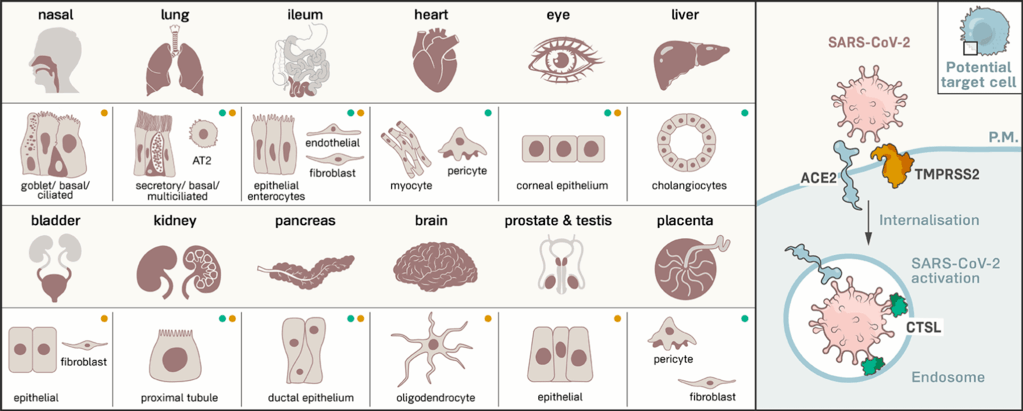
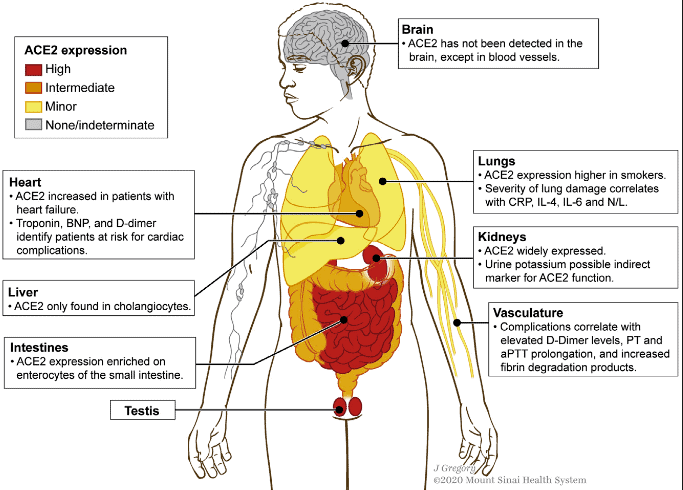
Spike protein from virus can bind to receptors on the human host cell surface: ACE2 (angiotensin-converting enzyme 2), and CD147 (also known as Basigin or EMMPRIN), mediating viral invasion and dissemination of virus among other cells.
ACE2 receptors are found on many types of cells, including those in the lungs, intestines, kidneys, and heart. The cell receptor CD147 is found on epithelial cells (the cells that line the surfaces of your body), which means they’re on your skin, blood vessels, urinary tract, uterus and organs, as well as on tumors.
The SARS-CoV-2 spike is 10 to 20 times more likely to bind to ACE2 on human cells than the spike from the SARS virus from 2002, which may enable SARS-CoV-2 to spread more easily from person to person than other coronaviruses.
You can see what parts of the body have the most ACE2 receptors in the depictions below. The virus needs these receptors, as well as CD147 receptors to infect you, and therefore will go where they’re most prevalent once they get past the respiratory tract.
During the early stages of infection, often called “incubation,” there are enough healthy (not yet hijacked and destroyed) cells to compensate for their fallen neighbors, but as the number of virus organisms in the body grows, the rate at which damage is being done also grows. Eventually, the healthy cells can no longer compensate for those infected and dead, and tissue and organ function becomes impaired.
This impact is experienced as “symptoms.”
Symptoms vary depending on the function of the cells that are damaged. In COVID-19, the virus infects the alveoli. Alveoli are the blood/lungs interface where oxygen passes from the lungs to the blood, and carbon dioxide passes from the blood to the lungs.
Without functioning alveoli, each respiration does not remove as much carbon dioxide from the blood or provide as much oxygen to the blood as it used to. To make up for the loss of efficiency per breath, the body is forced to undergo more respirations to provide the same oxygen supply.
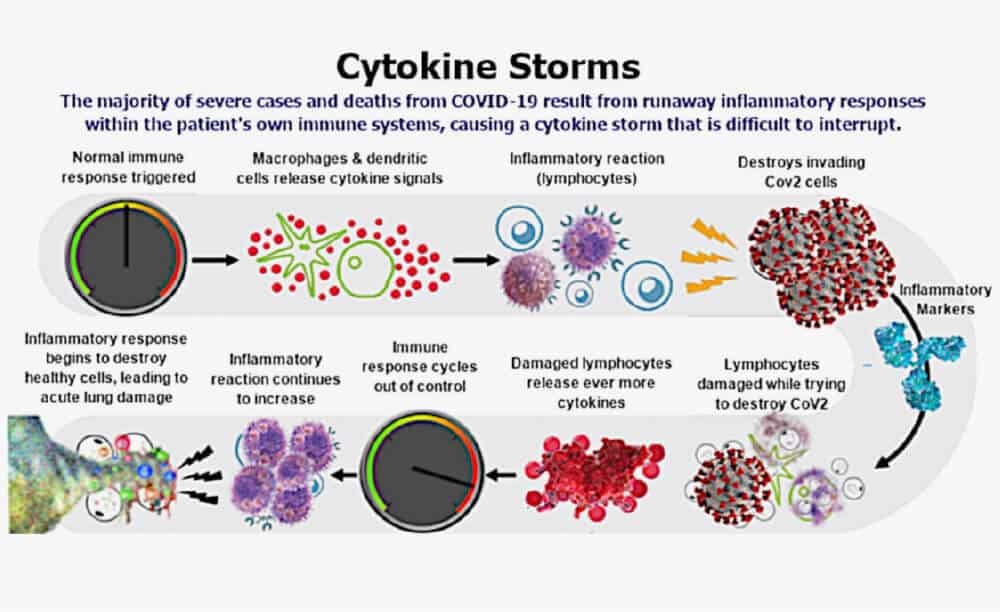
This is happening to the lungs, in part, due to excess inflammation that occurred from an overproduction of inflammatory signals from cytokines. If these cytokine immune signaling molecules are released at high levels, and responses like inflammation and immune activity wind up being poorly regulated, then the "cytokine storm” can happen.
The Cytokine Storm
A cytokine storm is the uncontrolled release of proteins that trigger a massive inflammatory response. This overreaction of the body’s natural immune defense can wreak havoc on vital organs. The cytokine storm doesn’t only affect the lungs: it often causes the immune cells to attack and inflame other organs including the kidneys, liver and heart.
These signaling cells also control the body’s clotting function, which means patients experiencing a cytokine storm are more prone to blood clots — putting them at greater risk of heart attack or stroke.
To analogize the cytokine storm, imagine an apartment building. One apartment catches on fire, an alarm goes off, and the apartment unit’s water sprinkler turns on. This is a good and appropriate response, but if all the sprinklers in all of the apartments in the building turn on, then there will be widespread water damage.
One apartment’s sprinkler is needed and appropriate, but all of them in the building getting turned on is an overreaction.
Unfortunately, people who are immunocompromised for some reason are more vulnerable to a cytokine storm. Their immune systems aren’t up to snuff due to age or some illness. In patients with severe cases of COVID-19, these cytokine storms can be life-threatening, and somehow block T and B cells from helping effectively.
To complicate matters, older people produce fewer new T and B cells, which means they have less of these cells available to fight new, unfamiliar viruses that they haven't encountered before.
In the case of SARS-CoV-2, everyone — even those who are asymptomatic — seem to have reduced levels of T cells.
This reduction is evident in two categories of T cells: T-killer cells that kill virus-infected cells, and T-helper cells that induce other immune cells to increase their activity.
But that’s not all.
With a SARS-CoV-2 infection, at the same time the number of T-killer and T-helper cells drop, immune signaling molecules linked to inflammation rise. This can lead to the hyperinflammatory state that can dramatically worsen your health.
It’s been well established that severe or fatal cases of COVID-19 are linked with hyperinflammation, which is a cause of organ damage, particularly in the lungs, which can lead to death.
Despite the potential of a cytokine storm, many infected people still clear the virus after a few weeks of nasty symptoms, and are therefore not in danger of hyperinflammation.
But others don’t. This could be because they inhaled a large dose of virus. Or perhaps their innate immune systems were already weakened through old age or chronic disease, the so-called comorbidities that I address in Lesson 10.
In some cases, the adaptive immune system also under-performs: T cells mobilize, but their levels recede before the virus is vanquished.
What can happen then is akin to an immunosuppressed state, whereby the immune system's ability to fight the virus is compromised, or entirely absent.
This could allow the virus to migrate deeper into the body. It could go, for instance, toward the vulnerable cells of the lungs, and to other organs including the kidneys, blood vessels, and the gastrointestinal and nervous systems.
In this case, the immune system can’t constrain the virus, but it doesn’t stop trying. And that’s also a problem.
It’s a problem because immune responses are violent. Cells are destroyed. Harmful chemicals are unleashed. This is necessary if that violence is targeted and restrained. But if an infection is allowed to run wild, the immune system might do the same thing -- it can, in effect, run wild too. If it does, it can cause much collateral damage as it tries and fails to control the virus.
Apparently, this is what happens in severe cases of COVID-19, where a person gets a double whammy -- because the virus isn’t cleared quickly enough, you’re susceptible to damage from the virus and the immune system.
COVID-19 Patient Profiles
An analysis of patients with COVID-19 admitted to a hospital revealed three distinct profiles that influenced the evolution and severity of COVID-19:
- The first profile was characterized by low expression of proinflammatory cytokines and adequate tissue repair genes. In this case, the disease remained moderate and led to eventual recovery.
- The second profile was characterized by highly elevated proinflammatory cytokines, worse disease and death.
- The third profile was similar to the second, only worse.
This is what may be happening to many patients in intensive-care units. They seem to succumb to the ravages of their own immune cells, even if they eventually beat the virus. Others suffer from lasting lung and heart problems, long after they are discharged from the hospital.
Right now, no one knows exactly why this happens, and why it happens only in some people. It’s still unclear, for example, why so many “long-haulers” have endured months of debilitating symptoms.
These are people who had COVID, and recovered from the worst symptoms, but experience long term side effects. Many of them have never been hospitalized, and so aren’t represented in existing studies that have measured antibody and T cell responses.
Now that you have a clear idea about how harmful a SARS-CoV-2 infection and resulting COVID-19 illness can be to your health, hopefully you're inspired to pay attention to the next protocol, which is all about prevention.
Your Takeaway
Remember these five things about SARS-CoV-2:
- This virus is a respiratory virus that infects you via the mouth, nose and eyes.
- It can spread undetected by your immune system for two days or longer, thereby spreading its infection to various tissues in the upper and lower respiratory systems and beyond.
- It can produce excess inflammation that can cause a dangerous hyperinflammatory condition called the “cytokine storm”.
- Some people can get infected and be asymptomatic, having no to few minor symptoms; whereas others can get deathly ill.
- The most vulnerable are the elderly and those with chronic illnesses. (See Lesson 10.)

Leave a comment
Comment as a guest: