Get The Right Gut Bacteria for Brain Health, Part 2: The “Gut-Brain” Axis
Do you have the right gut bacteria for brain health, so that you don’t experience dementia or Alzheimer’s as you get older? Learn how your gut affects your brain and which probiotics can help make keep your mind razor sharp. [Watch the video.]
Read Part 1AS DESCRIBED in this study, there’s currently a paradigm shift happening in what neuroscientists are learning about how our gut microbes affect our brains. They already know that those single-cell bacterium in our guts have an impact on our brain, but the holy grail will be to identify the gut bacteria for brain health, and the gut bacteria for brain illness.
These discoveries of the size and complexity of the human microbiome have resulted in an ongoing reevaluation of many concepts of health and disease, including diseases affecting the central nervous system, which consists of the brain and spinal cord and controls most functions of the body and mind.
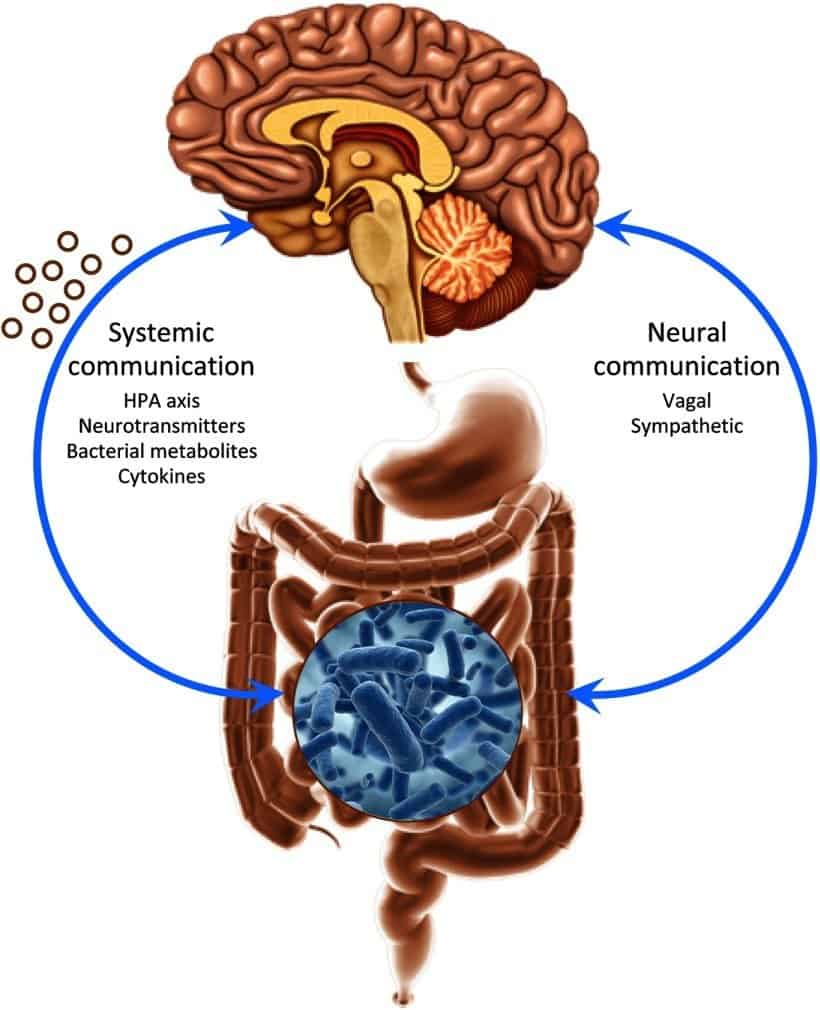
A growing body of preclinical literature has demonstrated that the brain and gut are connected via multiple neuroendocrine signalling mechanisms. (The neuroendocrine system is the mechanism by which the hypothalamus maintains homeostasis, regulating reproduction, metabolism, eating and drinking behavior, energy utilization, osmolarity and blood pressure.)
What this means is that changes to to the gut microbiome can affect emotional behavior and related brain systems, either for good or ill.
It’s now clear that alterations in the gut microbiome may play a disordered physiological processes associated with disease or injury (“pathophysiological role”), including autism spectrum disorder, anxiety, depression, and chronic pain.
In this article, you’ll discover:
- An overview about your brain/microbiome by everyone’s favorite online science show, SciShow;
- The SciShow video on the subject;
- How a diet rich in saturated fat and sugar affects the gut bacteria for brain health;
- A review of a study showing how antibiotics, like penicillin, destroy beneficial gut bacteria; and
- Which probiotic strains are the right gut bacteria for brain health.
Let’s dig in…
Your Brain/Microbiome Connection
The first thing to do is to get a good overview of what scientists are discovering about the role your microbiome plays in your overall health. For that I turn to SciShow.
If you’re one of the 4+ million subscribers to the SciShow on Youtube, or read my article, Heal Yourself and Become Superman with Specialized Probiotics, then you know about Hank Green and his SciShow posse.
The SciShow crew just made another video on about the microbiome, which I’ll summarize, as well as add some of my own commentary, including three graphs you’re about to see that underscore the importance of this topic. If you rather watch the video than read the summary, scroll down and do so.
Scientists now know that your microbiome plays a big role in your overall health, and that’s changing the way that doctors treat all kinds of conditions, from prescribing antibiotics to managing irritable bowel syndrome (IBS).
It makes sense that the microbes in your gut could play a role in your dietary and gastrointestinal health, but it does sound crazy that this gut microbiome can also affect your brain.
Your guts might have such a big influence on your brain that funding agencies are pouring millions of dollars into understanding what researchers are calling the microbiome-gut-brain axis. By learning more about this connection, scientists are hoping to better understand human mental health — and maybe even develop some new therapies along the way.
Why this matters to you in three graphs
Take a look at the following three graphs that depict how our cognitive capacities declines as we age. They should give you pause and underscore the need to stay vigilant with doing everything possible to maintain good cognitive health.
Cognitive Decline with Age
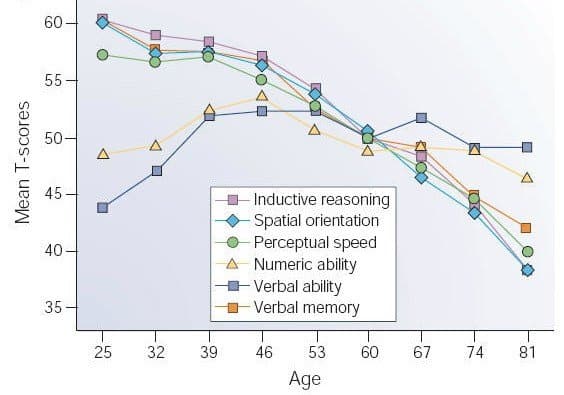 (source)
(source)
As the graph above shows, after the mid-forties, the various attributes associated with cognition decline. For many, the future doesn’t look any brighter given the prevalence of dreaded Alzheimer’s?
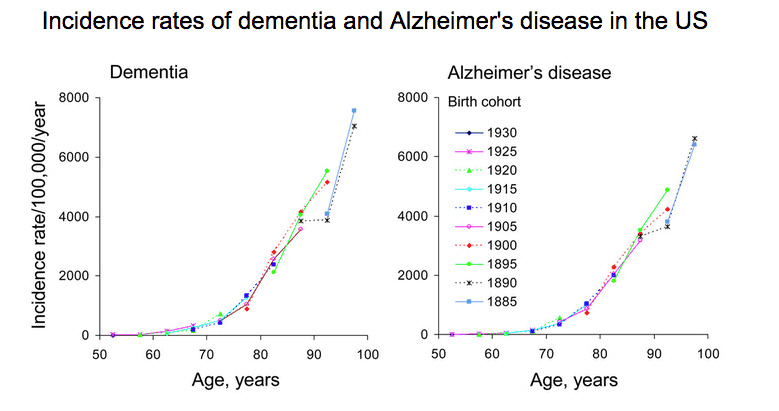 It’s not a pretty picture. It makes sense to do everything in our power to stay off those downward (in the first graph) and upward (in the second) curves.
It’s not a pretty picture. It makes sense to do everything in our power to stay off those downward (in the first graph) and upward (in the second) curves.
Ensuring that your microbiome is populated with the right beneficial bacteria is a major factor to maintain cognitive health. Read on to find out why.
Your gut is your second brain
 (source)
(source)
For years, researchers have been studying the enteric nervous system, or ENS, and its dynamic relationship with the central nervous system. It’s made up of more than 500 million neurons that control your guts.
Because our gut is connected to our central nervous system by our vagus nerve (which forms part of the involuntary nervous system and commands unconscious body procedures, such as keeping the heart rate constant and controlling food digestion), scientists new there was a connection between our gut and brain, thereby the reference to the gut as the “second brain”.
Despite this connection, scientists used to assume that the microbes in our gut couldn’t affect the brain because of the so-called “blood-brain barrier”, a semipermeable membrane barrier that separates the circulating blood from the brain’s extracellular fluid in the central nervous system.
The blood-brain barrier’s really important, because unlike an infection in your toe or on your skin, which aren’t usually life-threatening, brain infections tend to be pretty deadly. So your brain is structured to keep infections out.
Given that it’s hard for almost anything, including microbes (like gut bacteria) to get through the barrier (except in cases of serious injury or illness) neuroscientists presumed that gut bacteria in the gut microbiome. Turns out, they were wrong.
Your gut and psychological stress
Early research starting in the 1970s showed that stress could affect the kinds of microbes found in the guts of mice. One group found that stressing out mice by depriving them of food or water caused them to have more coliform bacteria, like E. coli, (you want less of that) and less of another kind of bacteria, called lactobacilli (you want more of that), in their intestines.
Another group found that the stress of dealing with an aggressive cage mate led to changes in the populations of other kinds of bacteria. But even though it was clear that stress could affect the kinds of microbes in the intestines, it wasn’t clear if it was a two-way relationship.
Could gut microbes be affecting psychological stress levels?
The first big breakthrough on this question came in 2004, when some scientists from Kyushu University in Japan discovered that exposure to certain kinds of microbes had dramatic effects on brain chemical levels.
For the study, the scientists used germ free mice mice that were delivered by C-section and immediately placed in a super clean cage that kept them unexposed to any microbes.
Compared to specific pathogen free mice — that is, mice that were exposed to a known set of microbes — the germ free mice got a lot more stressed out when they were restrained. Apparently, there was something about the bacteria in the mice was helping keep their stress levels in check.
The team found that the brains of the germ free mice had less of a protein called brain-derived neurotrophic factor, or BDNF. BDNF is important for learning, memory, and higher-order thinking, and the germ free mice had less of it in the brain regions that determine how an animal reacts to stress.
It’s not clear how microbes could be affecting BDNF levels, since it’s believed that they can’t cross the blood-brain barrier under normal circumstances. But something about the presence of bacteria in the gut seems to have a body-wide effect that leads directly to changes in brain chemistry.
The results of that study kicked off a bunch of new research projects to better understand the relationship between the microbiome and the brain, mostly using these germ free mice.
Some research from the early 2010s found that, while the germ free mice were more affected by certain kinds of acute stress, like restraint, they were less anxious about other kinds of stress — like being placed in a new environment. So it seems like the relationship between microbes and stress is complex, which was underscored by studies that indicate that mice without a microbiome aren’t always more sensitive to stress.
Such studies looked into what happens when you colonize germ free mice (no microbiome) with bacteria to observe whether their behavior changes, or how the bacteria affect certain stress-related genes in the brain.
In a study from 2011, one group of scientists found that exposing germ free mice to the microbiomes of other mice could influence their behavior. For instance would a shy germ free mouse do more exploring if it was implanted with microbes from a more adventurous mouse?
It did.
The behavioral changes corresponded to an increase in that BDNF protein, meaning that the microbiome transplant had direct effects on brain chemistry. So it’s clear that the microbiome does affect the brain.
Your microbes make some important neurotransmitters
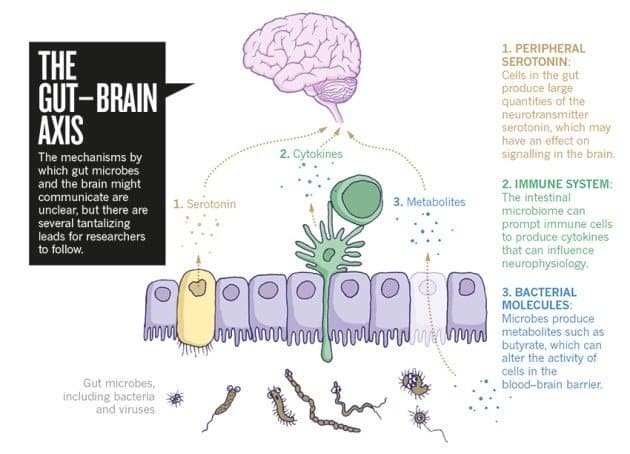 (source)
(source)
Take serotonin, for example.
Serotonin is a critical neurotransmitter primarily found in our gastrointestinal tract that is well known for influencing mood. Many drugs prescribed for depression and anxiety affect serotonin signaling in the brain even though most of our serotonin isn’t made in the brain.
Up to 80% of serotonin is made in your gut, and the microbes living there can affect how much serotonin is produced; thus changes in the numbers of microbes that produce serotonin could have big effects on overall levels of serotonin in your body, and could also affect your brain.
Even when they aren’t producing important neurotransmitters, microbes can trigger responses from the immune system, which in turn can have a big impact on the brain. The microbiome can affect the production of cytokines, which are proteins produced by immune system cells. Some of those proteins, like one called interleukin-6, are known to influence stress; unsurprising given what we learned about stress in the mice experiments touched on above.
Researchers have also discovered that microbes can release molecules that affect the behavior of the blood-brain barrier, like making it more or less permeable to outside molecules, which can affect what’s allowed in and out of the brain.
The germ free mice studies have been important and informative, but it’s hard to translate them to humans — even though about 97% of our DNA is the same, it’s unlikely that a human would accept being placed in a sterile, totally microbe-free bubble. Nonetheless, these studies do show that the microbiome has an effect on the brain, and they’re still useful because they give researchers total control over what kinds of bacteria the mice are or aren’t exposed to.
At this point, it’s clear that there’s a relationship between our microbiome and our mental health. Future studies are likely to explore:
- The exact probiotics and prebiotics (food for probotics) that influence mood. (See below.)
- Humanizing the mouse microbiome — basically, making the microbiomes of the mice more human-like by taking fecal transplants from both healthy and sick human patients and inserting them into mice to study the effects. That kind of experiment can let researchers pick apart how differences in the microbiome connect with changes in mental health.
- How other things that affect our microbiomes, like antibiotic treatments could affect our mental health and cognition. (See below.)
Without further adieu, watch SciShow’s Microbiome and the Brain, and then continue with how diet affects your microbiome and cognition, the perils of antibotics and a rundown of specific probiotics you can supplement with that might be useful for keeping your brain healthy as time ticks on.
Diet, Microbiome and Cognition Gut Bacteria for Brain Health
The open access online science publication, Frontiers, posted an article last January with a head-spinning title: Gut to Brain Dysbiosis: Mechanisms Linking Western Diet Consumption, the Microbiome, and Cognitive Impairment. It’s very sciency, but the information is important to know, so I’ll present some bullet points, and if any grab your interest, click on over to the article.
A diet high in saturated fat and added sugars negatively impacts cognitive function, in part due to emerging evidence that suggests such a diet significantly alters the proportions of commensal (the “good”) bacteria in the gastrointestinal tract.
The article reviews and highlights evidence that suggests:
- A high saturated fat, sugary diet negatively impacts neurocognitive function,
- Gut bacteria can alter intestinal permeability and blood brain barrier integrity, thus making the brain more vulnerable to the influx of harmful substances via circulation from the gut to the brain.
- Such a diet increases production of endotoxins (toxins created within the body) by commensal bacteria, which may promote neuroinflammation and cognitive dysfunction.
- Diet-induced alterations in gut microbiota impair peripheral insulin sensitivity (how readily body cells in your periphery tissue, such as muscle and fat, can absorb glucose).
- In some cases treatment with specific probiotics or prebiotics (food for probiotics, such as resistant starch) can prevent or reverse some of the deleterious impact of a high saturated/high sugar diet on neuropsychological outcomes, indicating that targeting the microbiome may be a successful strategy for combating dietary- and metabolic-associated cognitive impairment.
If your diet is less than stellar, you might want to dig into the details behind the bullet points presented above by reading the article.
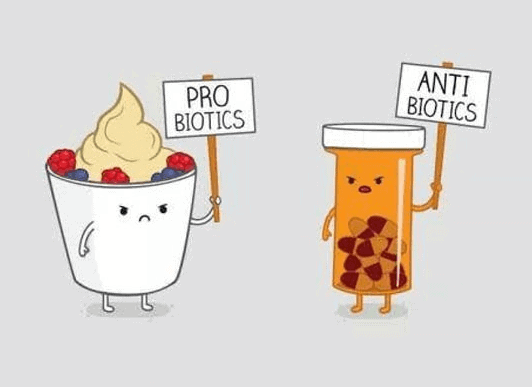
Beware Penicillin and Other Antibiotics
As you just learned, what kind of food you eat matters to the health of your microbiome, and thereby, to the health of your brain, but in these days of rampant antibiotic overuse it’s very important to realize that antibiotics and many other medications can destroy the beneficial bacteria in your gut.
A recent article, reviewed a mouse study run by Dr. Sophie Leclercq of McMaster University demonstrated that penicillin not only affects behavior changes (primarily anti-social) in the mother mice who get the penicillin, but to their offspring as well.
This particular study is unlikely to be reproduced in humans, since we don’t tend to be amenable to living in the sterile conditions that some of the mice cohorts were subject to in order to compare them to normally raised mice. Nonetheless, research on mice is prevalent because their DNA is 97% similar to ours, and thus there’s a good chance that they accurately model what would happen to humans under the same conditions.
When you take penicillin and other medications, make sure you also consume high quality probiotics for at least one month afterwards.
Which Probiotics Can Improve Your Gut Bacteria for Brain Health?
Now we return to where we started with that study about how our gut microbes affect our brains. The study points to a range of probiotics that have been investigated in animal models (mostly rodents it appears).
Here’s the upshot:
The probiotics Bifidobacterium and Lactobacillus show beneficial effects on anxiety- and depression-like behavior, but only in specific strains:
- Bifidobacterium infantis improved early-life stress-induced immune changes and depressive-like behaviors in adulthood. See PB8 Probiotic on Amazon.com
- Lactobacillus helveticus ROO52 has also been shown to reduce anxiety-like behavior and alleviate memory dysfunction. See Garden of Life Probiotic on Amazon.com
- Lactobacillus rhamnosus JB-1 reduced anxiety- and depression-related behaviors in the elevated plus maze and forced swim test, respectively. See Nexabiotic Advanced Probiotic on Amazon.com
- Mycobacterium vaccae reduced anxiety and improved performance on a complex maze task
- Bifidobacterium longum normalizes anxiety-like behavior in a colitis (inflammation of the inner lining of the colon) model. See Nexabiotic Advanced Probiotic on Amazon.com
I got your head spinning again, yes? Mine too.
What do you do with this information?
If any of the strains described above address your health concern, click on the Amazon link and see if the probiotic product(s) may be for you.
You may also check out Labdoor’s Top 10 laboratory tested and rated probiotics.
Lastly, read my article Heal Yourself and Become Superman with Specialized Probiotics where delve into the foods to eat that feed your beneficial bacteria and list the probiotic strains favored by Dr. David Williams, which are:
- L. acidophilus—This is the most important strain of the Lactobacillus species and, it readily colonizes on the walls of the small intestine. It supports nutrient absorption and helps with the digestion of dairy foods.
- B. longum—Like L. acidophilus, B. Longum is one of the most common bacteria found in the digestive tracts of adults, and it helps maintain the integrity of the gut wall. It is particularly active as a scavenger of toxins.
- B. bifidum—This strain, found in both the small and large intestine, is critical for the healthy digestion of dairy products. This is especially important as you grow older and your natural ability to digest dairy declines. B. bifidum also is important for its ability to break down complex carbohydrates, fat, and protein into small components that the body can use more efficiently.
Secondarily, Dr. Williamss likes:
- L. rhamnosus—Known as the premier “travel probiotic,” this strain can help prevent occasional traveler’s diarrhea.
- L. fermentum—This Lactobacillus strain helps neutralize some of the byproducts of digestion and promote a healthy level of gut bacteria.
This is Dr. William’s formulated probiotic product:
UPDATE: Just ran across a Life Extension supplement containing probiotics known to positively influence biochemical signaling between the gastrointestinal tract and the nervous system, with positive effects on mood, called FLORASSIST® Mood. The two bacterial strains are Lactobacillus helveticus strain R0052 and Bifidobacterium longum strain R0175. I haven’t used it, can’t vouch for it, but you may wish to learn more about it.
Your Takeaway
Remember these four things (and do three of them):
- Your gut is connected to your brain and thereby the bacteria in your gut (part of your microbiome) affects your brain and its ability to perform cognitively.
- What you eat and the drugs you take — particularly antibiotics — destroy the beneficial gut bacteria and enable the harmful bacteria to dominate and thrive. Reduce your consumption of saturated fat and sugar, not just added sugar, but the sugar that hides in most fast and packaged foods.
- Various probiotics have been identified to be the right gut bacteria for brain health, so do yourself a favor and choose a high quality probiotic supplement that contains as many of such bacteria as you can find.
Get your microbiome checked at uBiome. Update: they’re now out of business.
Read Part 1
Last Updated on October 16, 2019 by Joe Garma