Sleep and Healthspan: Part 1, The Problem

Sleep is a fundamental biological process that allows our bodies and minds to recharge. Odds are, yours is insufficient. Here’s why it matters, particularly as we age.

Credit: Mymichigan.org
What Is Sleep?
We all do it — sleep has been observed in mammals, birds, reptiles, amphibians, and some fish, and, in some form, in insects; and even in simpler animals such as nematodes (tiny worms).
So, what is it?
Sleep is a complex state characterized by altered consciousness, reduced responsiveness, and distinct brain activity patterns. It’s governed by an internal circadian clock that promotes sleep at night for diurnal organisms (such as humans), and in the day for nocturnal organisms (such as rodents).
Sleep is so natural, so common, so automatic that it’s a ritual we humans all share every night, but perhaps don’t give enough consideration, given its critical importance to our mental, emotional and physical states. Sleep is not merely a period of rest; it’s an active biological process vital for optimal physical and cognitive function. And all this activity occurs within three basic sleep cycles:
- REM,
- Light, and
- Deep sleep.
These three stages or cycles of sleep are referred to as “sleep architecture”.
Given how critically important sleep is to your healthspan, if you want to optimize it, you must learn:
- What are the common problems we encounter with sleep as we age, and
- What to do about it.
I’m going to answer #1 in this post, Part 1. In Part 2, I’ll answer “What to do about it” .
Let’s dig in…
The Importance of Sleep Architecture
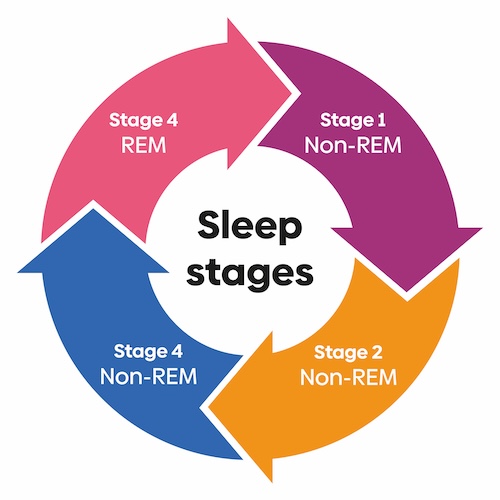
Sleep is not a uniform state; it comprises distinct stages, or cycles, with unique functions crucial for overall health. These different cycles rotate between Non-Rapid Eye Movement (NREM) and Rapid Eye Movement (REM) sleep.
Each cycle includes stages of light sleep (where we transition in and out of sleep), deep sleep (which is crucial for physical recovery and health), and REM sleep (important for cognitive functions and memory consolidation).
REM Sleep
(Duration: around 20-25% of total sleep time.)
During REM (Rapid Eye Movement) sleep, brain activity increases, becoming similar to wakefulness, while the body’s major muscle groups become paralyzed, but with rapid eye movements. In REM we dream, process emotions and learning, and consolidate memories.
- Most vivid dreaming occurs in REM. The dreams experienced in this stage tend to be more intense, emotional, and story-like compared to the fragmented thoughts and images that may occur during other stages of sleep.
- This sleep stage is essential for memory consolidation, emotional processing and learning. Memory consolidation is the process by which new information and experiences are transformed from short-term memories into stable, long-term memories. This includes both declarative memories (facts and events) and procedural memories (skills and habits). The heightened brain activity and unique brain wave patterns during REM are thought to facilitate the strengthening and integration of these memories into long-term storage.
- REM sleep is believed to be important for the processing and integration of emotional memories. The emotional intensity of dreams during REM sleep may help the brain process and make sense of emotionally significant experiences.
- By supporting both dreaming and memory consolidation, REM sleep contributes to cognitive functions such as learning, problem-solving, and emotional regulation. Disruptions in REM sleep have been linked to impairments in memory, mood, and overall cognitive performance.
- While the exact mechanisms are still being studied, the dreaming and memory consolidation functions of REM sleep highlight the importance of this stage for overall cognitive health and well-being.
Light Sleep
(Duration: around 50-60% of total sleep time.)
Light sleep serves as an important transition period allowing the body to relax and reach deeper stages of restorative sleep.
Light sleep has two stages, Stage 1 and Stage 2, and has these characteristics [1][3]:
- Transitional state from wakefulness to sleep (Stage 1).
- Slowing of brain wave activity with lower amplitude and higher frequency waves (Stage 2).
- Appearance of brief bursts of rapid brain wave activity called sleep spindles and K-complexes (Stage 2).
- Muscle tone remains relatively unchanged from wakefulness, with occasional small muscle twitches.
- Heart rate and breathing become more regular and slowed compared to wakefulness.
- Body temperature drops slightly.
- It’s easier to be awakened from light sleep compared to deep sleep.
- While some fragmented thoughts or imagery may occur, significant dreaming is rare during light sleep stages.
Deep Sleep
(Duration: around 20-25% of total sleep time.)
Deep sleep, also known as slow-wave sleep or NREM (non-rapid eye movement) Stage 3, is the most restorative stage of sleep, and is crucial for physical and cognitive restoration, as it helps the body recover from daily wear and tear, promotes growth and repair, and supports memory consolidation processes.
Insufficient deep sleep can lead to fatigue, impaired cognitive function, and other health issues. Unfortunately, the amount of time spent in deep sleep declines with age, therefore, finding ways to prolong or improve deep sleep in the elderly could potentially help optimize health span and overall well-being.
Here are some key attributes of deep sleep [3][4][5]:
- Deep sleep is characterized by high-amplitude, low-frequency brain waves called delta waves. These slow brain waves are the slowest and highest in amplitude compared to other sleep stages.
- There are no rapid eye movements during deep sleep.
- Muscle tone is significantly reduced during this stage, making it difficult to awaken someone from deep sleep.
- Breathing and heart rate are at their slowest and most regular during deep sleep.
- Blood pressure drops during deep sleep, providing a rest for the cardiovascular system.
- The pituitary gland releases growth hormone during deep sleep, which is essential for growth and repair of tissues and muscles.
- While not as important for memory consolidation as REM sleep, deep sleep plays a role in strengthening and integrating new memories with existing knowledge.
- The need for deep sleep increases with sleep deprivation, as it is the most restorative stage of sleep.
- It’s very difficult to wake someone from deep sleep, as the arousal threshold (the amount of stimulation required to wake up) is highest during this stage.
The bottom line here is that we sleep within each of these cycles, and we want each cycle to last the amount of time needed to obtain restorative sleep. Unfortunately, other than feeling great every morning that you wake up, with all your health metrics in optimum ranges, you can’t intuit how much time you’re sleeping in each sleep stage. Although not completely accurate, what can help is a smart watch, band or ring that tracks sleep. If you have one, use it!
Time Asleep Is Impacted by Age, Circadian Rhythms and Lifestyle Factors
Credit: Okoa.org
The ideal amount of sleep recommended varies across different age groups [6][7][8]. Let’s examine this through the lens of developmental needs, sleep architecture, lifestyle factors, circadian rhythms, along with some sleep attributes pertaining to older folks.
Recommended total sleep duration by age group:
- Adults 65+ years old: 7-8 hours per night
- Adults (18-64 years old): 7-9 hours per night
- Teenagers (14-17 years old): 8-10 hours per night
- School-aged children (6-13 years old): 9-11 hours per night
- Preschoolers (3-5 years old): 10-13 hours per night
- Toddlers (1-2 years old): 11-14 hours per night
- Infants (4-12 months old): 12-16 hours per night
Note that adults 65 and older (first bullet point above) tend to need a bit less sleep compared to younger adults. This is because as people age, the body’s circadian rhythms and sleep patterns change, as you’ll soon see.
Developmental needs
Sleep plays a crucial role in growth and development, especially in infants, children, and adolescents. During these stages, adequate sleep is essential for proper physical, cognitive, and emotional development.
Infants and young children require more sleep to support rapid brain development, growth spurts, and the formation of neural pathways. As individuals progress through childhood and adolescence, their sleep needs gradually decrease, but still remain higher than those of adults.
During adolescence, there is a natural shift in the circadian rhythm, leading to a tendency for later bedtimes and wake times. This shift is thought to be influenced by hormonal changes during puberty.
Lifestyle factors
Sleep needs can also be influenced by lifestyle factors, such as physical activity levels, stress, alcohol, exposure to environmental factors like light and noise, etc. These factors can vary across age groups, further contributing to differences in recommended sleep durations.
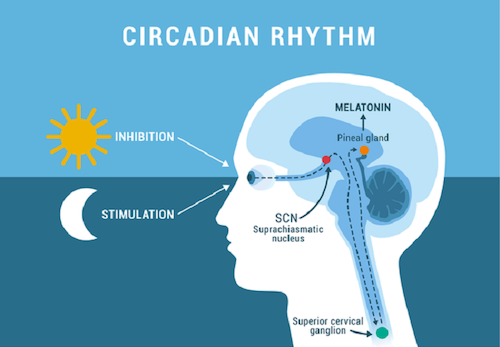
Circadian rhythm changes
The circadian rhythm is the internal clock found in every organ. It functions to regulate your sleep-wake cycle, as guided by something called the SCN (suprachiasmatic nucleus), a tiny group of neurons located in the brain’s hypothalamus. This is done by the SCN’s daily programming of organismic functions by regulating day-to-day oscillations of the internal milieu and synchronizing them to the changing cycles of day and night and of body state [9].
The phrase “day-to-day oscillations of the internal milieu” refers to the cyclical fluctuations or rhythmic changes that occur within the internal physiological environment of the body on a daily basis.
The “internal milieu” refers to the complex set of conditions and substances present inside the body, such as hormone levels, body temperature, metabolism, and other physiological processes.
Many of these internal processes exhibit natural oscillations or rhythmic patterns that follow a roughly 24-hour cycle, also known as circadian rhythms. The SCN coordinates and controls these daily rhythmic fluctuations in various physiological processes and conditions within the body.
I’m going into some detail here, because your “clock” affects a lot of your physiology, such as:
- Hormone secretion patterns (e.g., melatonin, cortisol)
- Body temperature variations
- Metabolic rate changes
- Sleep-wake cycles
- Digestive processes
- Immune function fluctuations
By regulating these day-to-day oscillations, the SCN ensures that the internal physiological processes are synchronized with the external cycles of day and night, as well as changes in the body’s state (e.g., awake, asleep, active, resting).
Our circadian clocks change throughout our life. Newborns and infants have a less established circadian rhythm, which becomes more regular as they age.
During adolescence, there is a natural shift in the circadian rhythm, leading to a tendency for later bedtimes and wake times. This shift is thought to be influenced by hormonal changes during puberty.
As we age, however, we tend to sleep less as our circadian rhythms change.
There are common changes in circadian rhythms that can impact sleep patterns and overall health when we get older. If not addressed properly, these changes can have implications for healthspan.
Circadian Rhythm Changes in Older Adults
- Advanced Sleep-Wake Cycle: Older adults tend to experience an advanced sleep-wake cycle, meaning they feel sleepy earlier in the evening and wake up earlier in the morning compared to younger adults. This shift is often referred to as a “morning” chronotype.
- Decreased Melatonin Production: The pineal gland’s production of melatonin, the hormone that regulates sleep-wake cycles, decreases with age. This can make it more difficult for older adults to fall asleep and maintain sleep quality throughout the night.
- Increased Sleep Fragmentation: Older adults are more prone to experiencing fragmented sleep, with frequent awakenings during the night. This can be due to various factors, including medical conditions, medication use, or changes in sleep architecture.
Circadian Rhythm Impact on Healthspan
These circadian rhythm changes can have a significant impact on the healthspan of older adults:
- Increased Risk of Sleep Disorders: The disruption in circadian rhythms can contribute to the development or exacerbation of sleep disorders, such as insomnia or sleep apnea, which can further impact overall health and quality of life.
- Cognitive Impairment: Sleep disturbances and circadian disruptions have been linked to an increased risk of cognitive decline, including Alzheimer’s disease and other forms of dementia.
- Metabolic Disturbances: Circadian misalignment can affect metabolic processes, increasing the risk of obesity, type 2 diabetes, and other metabolic disorders.
- Cardiovascular Issues: Sleep disturbances and circadian rhythm disruptions have been associated with an increased risk of hypertension, heart disease, and stroke.
- Mood Disorders: Changes in circadian rhythms and sleep patterns can contribute to the development or worsening of mood disorders, such as depression and anxiety.
Turns out, our circadian clocks are linked to sleep architecture.
Sleep architecture
The composition of sleep stages (REM, light and deep sleep), known as sleep architecture, also varies with age. And there is a direct relationship between the changes in circadian rhythms that occur with aging and the changes observed in sleep architecture among older adults.
As people age, the amount of time spent in deep sleep decreases, while the time spent in lighter stages of sleep increases. This shift in sleep architecture as we get older is natural, but not ideal.
As we age, the circadian rhythm (the internal clock that regulates the sleep-wake cycle) undergoes specific changes. These changes in circadian rhythms are closely linked to the alterations in sleep architecture, which you may remember, refers to the distribution and patterns of different sleep stages throughout the night.
There are at least four noteworthy circadian rhythm changes that relate to sleep architecture changes in the elderly [10][11][12][13]:
- Advanced Sleep-Wake Cycle. The tendency for older adults to experience an advanced sleep-wake cycle, where they feel sleepy earlier in the evening and wake up earlier in the morning, is directly tied to shifts in the circadian rhythm. This can lead to shorter total sleep times and an increased likelihood of early morning awakenings.
- Decreased Melatonin Production. The age-related decrease in melatonin production, a hormone that plays a crucial role in regulating circadian rhythms, can contribute to the disruption of sleep architecture. Melatonin is important for initiating and maintaining sleep, and its reduction can lead to more fragmented sleep and less time spent in deep, restorative sleep stages.
- Changes in Sleep Stage Distribution. Older adults tend to spend less time in deep, slow-wave sleep and REM sleep, which are the most restorative stages of sleep. This change in sleep architecture is closely tied to the circadian rhythm disruptions that occur with age, as the body’s internal clock plays a role in regulating the timing and distribution of different sleep stages.
- Sleep Fragmentation. The increased sleep fragmentation, with frequent awakenings during the night, that is common in older adults is partly due to the disruption of circadian rhythms. These disruptions can interfere with the normal sleep-wake cycle and contribute to more frequent arousals and difficulty maintaining consolidated sleep periods.
The age-related changes in circadian rhythms and the body’s internal clock are believed to be a significant contributing factor to the alterations in sleep architecture observed in older adults. But there are several other reasons why sleep can be disrupted as we get older, thereby potentially affecting health and longevity. I will address those disruptors and what to do about them in Part 2.
At this point you have a good idea about what constitutes sleep and what goes on within each sleep cycle. Now, let’s get a handle on the specific physiological impacts influenced by sleep, or the lack thereof.
Sleep’s Role in Physiological Health

Credit: Sequencewiz.org
We’ve all experienced the aftermath of a terrible night’s sleep — basically, a lousy day where our thinking is muddled, physical energy is compromised and mood is irritable. If this happens once in a while, there are no consequences to face; however, if chronic, then you’re going to get a lot less out of life.
That’s because you very much need what sleep does. During sleep the body undergoes various restorative processes, including tissue repair, muscle growth, and the release of hormones that regulate growth and appetite. Sleep also supports immune function by producing cytokines that fight inflammation and infection.
In this section, I’ll tell you about how dysregulated sleep can affect just about all of our physiological systems, such as:
- Cognition, memory and learning
- Metabolic regulation and weight management
- Immune system function
- Hormonal regulation
- Cardiovascular health
We will begin with cognition, because without that you won’t care about anything else.
Cognition, memory and learning
Sleep, particularly the REM stage, plays a crucial role in the brain’s memory consolidation, the process by which short-term memories are transformed into long-term memories. It also facilitates learning and cognitive performance by allowing the brain to process and integrate new information.
Some of this happens during deep sleep when the glymphatic system becomes more active. The glymphatic system is a recently discovered macroscopic waste clearance system that promotes efficient elimination of soluble proteins and metabolites from the central nervous system. This allows the brain to clear out waste products and toxins accumulated during wakefulness.
The glymphatic system is a macroscopic, brain-wide metabolic waste clearance system that operates during sleep. It’s a functional waste clearance pathway that facilitates the efficient elimination of soluble proteins and metabolites, including adenosine, from the central nervous system and brain interstitial space.
Here’s how it works:
- During wakefulness, the brain’s metabolic activity generates metabolic waste products, including adenosine, which accumulate in the interstitial spaces surrounding the brain cells.
- During sleep, the glymphatic system becomes more active. Cerebrospinal fluid (CSF) is pumped into the brain tissue, flushing out the accumulated metabolites, including adenosine, from the interstitial spaces.
- The waste products are then cleared from the brain tissue via perivascular spaces surrounding the cerebral blood vessels, ultimately draining into the systemic circulatory system for elimination from the body.
Sleep also facilitates neurogenesis (the creation of new neurons) and helps balance neurotransmitters that affect mood and cognition. When neurotransmitter balance is restored, memory consolidation and learning is enhanced.
When chronically deprived of sleep, there’s an increased risk of neurodegenerative diseases like Alzheimer’s and dementia. Studies suggest that insufficient sleep disrupts the brain’s ability to clear amyloid plaques, a hallmark of Alzheimer’s disease [14].
Metabolic regulation and weight management
Sleep deprivation has been linked to an increased risk of obesity and metabolic disorders, such as type 2 diabetes [15].
During sleep, the body regulates the release of hormones like leptin and ghrelin, which control appetite and satiety. This can negatively affect appetite regulation and metabolism.
Insufficient sleep can impair glucose metabolism and insulin sensitivity, increasing the risk of developing type 2 diabetes. Sleep disruptions can also exacerbate complications in individuals with existing diabetes.
Immune system function
Sleep is essential for maintaining a robust immune system [16]. Immune cells release cytokines during deep sleep. Cytokines are proteins that help fight infection and inflammation, thereby promoting healing and defense against infections.
Chronic sleep deprivation can weaken the immune response, increasing susceptibility to illness [17].
Hormonal regulation
Sleep regulates the release of hormones like growth hormone, which is essential for cell repair and tissue growth, and insulin, which controls blood sugar levels [x]. Disrupted sleep patterns can lead to various other hormonal imbalances, such as thyroid disorders. An imbalance in thyroid hormone levels can also disrupt sleep patterns [18].
High cortisol levels due to chronic stress can also interrupt the natural sleep cycle, reducing the proportion of deep and REM sleep. Stress can keep the body in a heightened state of alertness, and make it difficult to fall asleep or stay asleep, which is also stressful. This creates a vicious cycle as sleep deprivation further exacerbates stress [19].
Cardiovascular health
Chronic sleep deprivation or poor sleep quality has been associated with an increased risk of hypertension, heart disease, and stroke. Sleep plays a role in regulating blood pressure, inflammation, and other factors that contribute to cardiovascular health [20]. Restorative sleep allows the cardiovascular system to rest and repair.
Your Takeaway
Remember these three things:
- You can’t have good health, especially as you get older, without consistent restorative sleep wherein your sleeping pattern maintains the recommended time periods in each cycle: REM, light and deep sleep.
- If you can track your sleep cycles with a smart watch, band or ring, do so, and ensure that you consistently are in line with these ranges:
- REM: 20-25% of total sleep time
- Light: 50-60% of total sleep time
- Deep: 20-25% of total sleep time
- Chronic insufficient sleep can negatively impact cognition, metabolism, immunity, hormones and cardiovascular health. Since you have to do it anyway, do your best to get enough restorative sleep.
In Part 2, we’ll investigate specific sleep disruptors, such as sleep apnea, blue light and late night eating. I’ll tell you how they tie-in to the sleep cycle architecture and physiological conditions affected by sleep. After that, we’ll take a look at various protocols that can promote restorative sleep.
Go to Part 2
Last Updated on May 12, 2024 by Joe Garma


