What’s Your COVID Risk Level? Take the Test!

You will want to know your COVID risk level as we re-emerge from our homes and engage society once again, because this is going to give us greater exposure to the virus. Know your risk and take appropriate actions.
Check out my Covid Immunity CourseIn a general sense, you have a decent idea of your COVID risk level if you’ve been paying attention to news about this pandemic. I’m referring, of course, to a coronavirus called SARS-CoV-2 (severe acute respiratory syndrome coronavirus 2), the virus that causes the COVID-19 disease (coronavirus disease 2019). And if you do the hand washing, mask wearing, social distancing dance; are aware of the prevalence of the virus in your neighborhood; know your age; and have accounted for any chronic illness you might have — then you have a decent idea of your COVID risk level.
But let’s give it a score!
I’ll get to that in a minute, but first, a bit about COVID-19 and our immune system. This is an important bit because for too many people, this novel coronavirus confuses our immune system response to it, and impacts us in unanticipated ways.
How people’s health are affected by SARS-CoV-2 is all over the map — from those who don’t even know they have it (“asymptomatic”), to those who get put on ventilators and die. Even though we know that some cohorts, like the young, have less of a chance of getting infected and suffering from it, some do. And even though older people statistically have a much greater chance of getting really sick and even dying from COVID-19, many don’t.
The two basic, underlying common denominators behind the severity of COVID-19 are:
- The ability of your immune system to modulate its response to the SARS infection; and
- The presence and severity of certain comorbidities.
Let’s dive into what the medical establishment has learned so far about how our immune system responds to the SARS-CoV-2 virus and resulting COVID-19 disease, how certain comorbidities, such as heart disease and diabetes, compound the risk of infection and severity of the disease, and finally how you can test your COVID risk level.
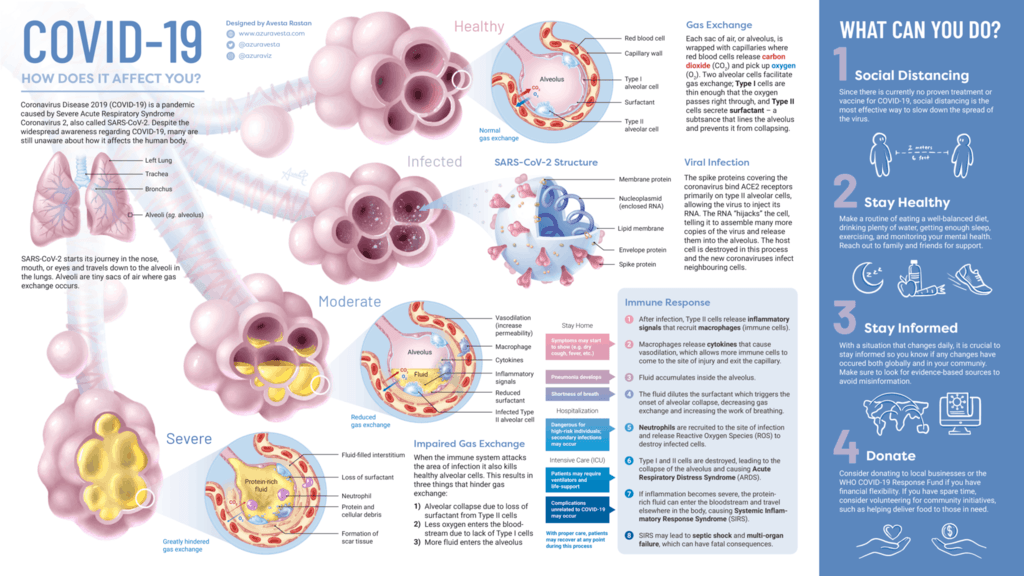
SARS-CoV-2, COVID-19 and Our Immune System Response
This virus messes with the typical way our immune system response to infection, and whatever resulting disease pathologies might occur. One simple reason for this is that SARS-CoV-2 virus is “novel”.
Perhaps you’ve seen that word used to describe COVID: “novel coronavirus COVID-19”, which conveys that this particular coronavirus, COVID-19, is novel, or new. What that means to our immune system is, “don’t know what this is, have no memory of it, not sure how to react”.
Our immune system is bewilderingly complex. Scientists don’t currently know enough about why the immune system of many people who get really sick from COVID-19 take too long to react to infection, and then overreact. [1,2,3,4]
But sometimes it does overreact and creates the dreaded “cytokine storm.”
With a typical respiratory virus, the body’s first line of defense, the innate immune response, starts right after the infection, like an infantry going after a foreign invader, killing the virus and any cells damaged by it. The second line of defense, the adaptive immune response, kicks in days later if any virus remains, employing what it has learned about the virus to mobilize a variety of special forces such as T cells and B cells.
A typical respiratory flu virus is a fast-moving infection that attacks certain target cells on the surface of the upper respiratory system and kills almost all of the target cells within two to three days. The death of these cells deprives the virus of more targets to infect and allows the body’s first line of defense, the innate immune response time to clear the body of almost all of the virus and any cells damaged by it before the adaptive system comes into play. In this instance, by the time the adaptive immune response kicks in (usually days later), if any virus remains, it can mobilize a variety of special forces such as T cells and B cells that are specifically tuned to fight that particular flu.
In the case of COVID-19, which targets surface cells throughout the respiratory system including in the lungs, the average viral incubation is six days, a much slower disease progression that other coronavirus. Mathematical modeling suggests that the adaptive immune response may kick in before the target cells are depleted, slowing down the infection and interfering with the innate immune response’s ability to kill off most of the virus quickly. [5]
Weiming Yuan, associate professor in the Department of Molecular Microbiology and Immunology at the Keck School of Medicine of USC says:
The danger is, as the infection keeps going on, it will mobilize the whole of the adaptive immune response with its multiple layers. This longer duration of viral activity may lead to an overreaction of the immune system, called a cytokine storm, which kills healthy cells, causing tissue damage.
The interaction of the innate and the adaptive immune responses might also explain why some COVID-19 patients experience two waves of the disease, appearing to get better before eventually getting much worse. What might be happening in this case is that the combined effect of the adaptive and the innate immune responses may reduce the virus to a low level temporarily; however, if the virus is not completely cleared, and the target cells regenerate, the virus can take hold again and reach another peak.
Those people who are asymptomatic or experience minor symptoms typically have an immune system that properly modulates between the innate and adaptive responses, such that the adaptive response is not exaggerated, bringing on hyperinflammation coincident with the cytokine storm.
As I wrote in my article, Make Your Immune System Smart, a cytokine is a short-lived signaling molecule that the body can release to activate inflammation in an attempt to contain and eradicate a virus. In a cytokine storm, the immune system floods the body with much more of these molecules than is necessary; so much more, in fact, that the level of excess inflammation becomes life threatening.
When this happens, a strong immune system response has become the villain, and the priority for doctors shifts from wanting a person’s immune system to fight off the virus to working to downregulate the immune response so it doesn’t kill the person or cause permanent organ damage. The challenge is striking a balance where neither the cytokine storm, nor the infection runs rampant.
Comorbidities Influence COVID-19 Severity
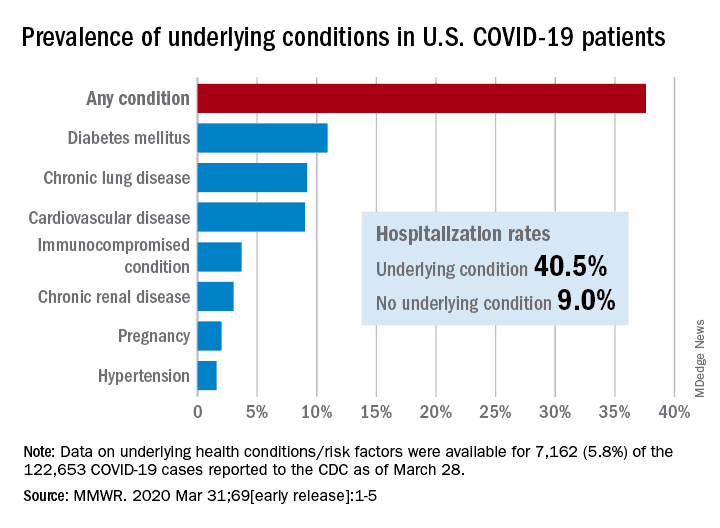 A “comorbidity” is the simultaneous presence of two chronic diseases or conditions in a person. People who have health issues, like heart disease, diabetes, obesity, or some lung disorder — or are over 60 years old — have a higher COVID risk level and a greater chance of getting very ill.
A “comorbidity” is the simultaneous presence of two chronic diseases or conditions in a person. People who have health issues, like heart disease, diabetes, obesity, or some lung disorder — or are over 60 years old — have a higher COVID risk level and a greater chance of getting very ill.
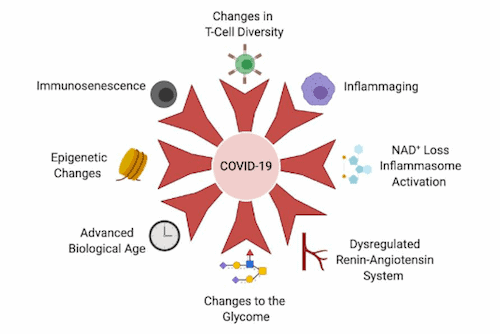
The common denominator between these particular comorbidities might be age.
Typically, it takes time for a chronic disease to become significantly deleterious to your health. So, for instance, a young adult who regularly over consumes high-sugar/carb foods might have high blood sugar, but perhaps in the prediabetic range. Over time, as you get older, that food consumption pattern keeps pushing the blood sugar up and impairing insulin efficiency, until type-2 diabetes sets in, typically alongside obesity.
Famed anti-aging geneticist, Dr. David Sinclair, and two of his associates, wrote a research paper about why COVID-19 disproportionately affects older people. They write that the ability to control viral load is one of the best predictors of whether a person will have mild or severe COVID-19symptoms. For the immune system to effectively suppress then eliminate SARS-CoV-2, it must perform four main tasks: (1) recognize, (2) alert, (3) destroy and (4) clear. Each of these mechanisms are known to be dysfunctional and increasingly heterogeneous in older people.
As we age, our immune system changes in two major ways:
- One is a gradual decline in immune function called immunosenescence, which hampers pathogen recognition, alert signaling and clearance. (This is not to be confused with cellular senescence, an aging-related phenomenon whereby old or dysfunctional cells arrest their cell cycle and can become epigenetically locked into a pro-inflammatory state in which they secrete cytokines and chemokines.)
- The other classic immune system change during aging is a chronic increase in systemic inflammation called inflammaging, which arises from an overactive, yet ineffective alert system.
For more detail about how aging is perhaps the most significant factor influencing COVID-19 health outcomes, read Dr. Sinclair’s paper.
And now onto an interesting test of your COVID risk level.
What’s Your COVID Risk Level?
Many nations are now telling their citizens that they can venture from their homes and re-engage in society with certain limitations, such as wearing masks and social distancing. As this is happening, there are already reports of a resurgence of infections. It’s likely that as more of us leave our protective homes with more regularity, we will be more exposed to infection, thereby increasing our COVID risk level.
That said, my COVID risk level is not yours. We may live in different places that have different numbers of infections. We may have different comorbidities, or none.
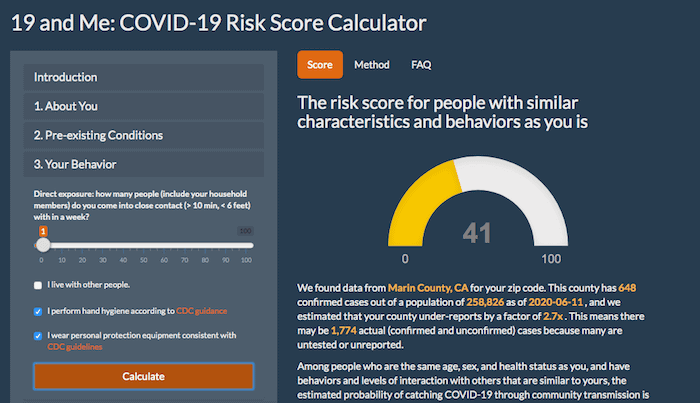
Recognizing this, a partnership between Mathematica and 23andMe built an app that can give you a decent estimate of your COVID risk level (actually, the risk of those with similar attributes) of contracting COVID-19 if you live in the U.S.
Because many important aspects of this disease remain unknown or uncertain, the app might not account for some information specific to you, your health status, and your behaviors that would be necessary to most accurately quantify your individual risk score. That said, an imperfect estimate, based on the best scientific evidence currently available, is better than no estimate. Your COVID risk level score may be just the thing you need to convince you to redouble your efforts to remain uninfected.
The app is divided into three sections:
1. About You
This section collects user input about geographic location, age, and gender.
Most of the public data on COVID-19 cases, such as the Johns Hopkins University Center for Systems Science and Engineering and the New York Times database, are available only at the county level in the USA. To get more definitive, the app has a built-in ZIP-code-to-county crosswalk using a publicly available Application Programming Interface (API) from the U.S. Department of Housing and Urban Development.
The app asks for age and biological sex because the risk of hospitalization and severe health outcomes from contracting COVID-19 also depends on these factors.
It uses the latest epidemiological evidence from the Chinese Center for Disease Control and Prevention (CDC), the U.S. CDC, and peer-reviewed articles to estimate how age and biological sex affect risk.
2. Pre-Existing Conditions
The next step asks if you have flu-like symptoms, and what underlying medical complications you may have. The algorithm has different methods to calculate the probability of someone having COVID-19 for those with and without flu-like symptoms. The underlying medical complications are important because they also determine the risks of developing a severe case of COVID-19, being hospitalized, and dying.
3. Your Behavior
Many risk factors for COVID-19 (place of residence, age, biological sex, and underlying medical conditions) cannot be easily modified, but there are things we all can do to mitigate our own risks. In this section of the app, you can estimate the number of people that you and your household members come into close contact with on a weekly basis. This input will feed into the calculation of the probability of contracting COVID-19. The U.S. CDC has recommended additional risk mitigation measures, such as hand washing and wearing personal protective equipment. Users can select check-boxes for these behaviors in the app to see how adopting these behaviors can reduce risk.
Your COVID Risk Level Score
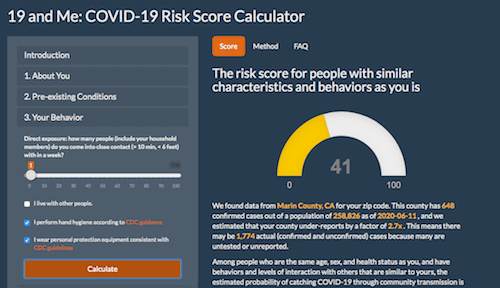
This is a screen shot of my (Joe Garma) COVID risk level test score. A score of 41 is good, but is only that high due to age, as I have no health issues, live alone and implement the CDC guidelines.
Mathematica and 23andMe designed the risk score like a credit score — a semi-quantitative metric that can be used to inform actions.
They centered the score around 50. If the risk score is between 1 and 30, you get a message saying the level of risk for people with similar characteristics and behavior is currently low, but to review the CDC planning guidance to make sure you’re prepared.
If the risk score is between 30 and 70, users are directed to the CDC resources on how to protect themselves and others from COVID-19. If the risk score is above 70, the message lets you know that the COVID risk level is serious and encourages sequestration, good hygiene, and to read additional CDC resources on disease prevention.
Here’s a screencast of me demonstrating how to take the COVID risk test:
Last Updated on September 29, 2022 by Joe Garma