I’ve Got COVID-19 — It’s Surging, Here’s What To Do

I’ve got COVID-19. It’s surging across the USA. I’ll tell you how it happened, and what I’m doing about it.
I’ve got COVID-19.
Yes, despite having been vaccinated for SARS-CoV19, along with two booster shots, the darn virus caught me.
I’ve got COVID-19 because I’ve been complacent.
For most of us, COVID is in the rear-view mirror. We are living our life as before the pandemic. I recently rejoined the gym that I left when COVID struck its mighty blow. That might have been my undoing. This is conjecture, but gym-going has been the only new thing added to my life recently, and guess what — there’s people there breathing hard and touching things.
Anyway, I should have been paying attention to what’s going on. A COVID-19 resurgence is going on.
The aim of this post is to:
- Alert you about a resurgence of COVID infections in the USA,
- Tell you my COVID story,
- Reveal the most significant vulnerability for infection, and
- Science-backed nutraceutical support.
Let’s dig in…
The COVID-19 Resurgence
Well before COVID existed, winters brought a spike in the number of people who got the cold and flu. This winter when incidences of all of these respiratory tract infections are rising, how can you tell when you start feeling lousy whether the cause is the cold, flu or COVID?
The fast answer is that unless you’re an experienced medical professional, you probably can not determine whether your symptoms are a result of the cold, flu or COVID infection. This is because the symptoms caused by these maladies can overlap.
Nonetheless, there are some helpful pointers worthy of mention.
Common cold
- Symptoms: Runny or stuffy nose, sneezing, sore throat, mild cough, headache, maybe mild fatigue.
- Usually less severe: Symptoms are milder than the flu or COVID.
- Gradual onset: Symptoms develop gradually over 1-3 days.
- Normal or slightly elevated temperature: Fever is uncommon or mild.
- Loss of taste/smell: Not typically associated with common cold.
Flu
- Symptoms: Fever, chills, muscle aches, headache, fatigue, dry cough, sore throat, runny or stuffy nose.
- Sudden onset: Symptoms come on suddenly within 1-4 days.
- High fever: Fever is often high (100°F or higher).
- Loss of taste/smell: Not typically associated with flu.
COVID-19
- Symptoms: Fever, cough (dry or with phlegm), fatigue, shortness of breath or difficulty breathing, loss of taste or smell, sore throat, muscle aches, headache, chills, runny or stuffy nose, diarrhea, nausea or vomiting.
- Variable onset: Can be gradual or sudden.
- Fever may be present or not: Fever is not always present, and can be moderate.
- Loss of taste/smell: More common than with cold or flu.
Dr. Andrew Huberman Explains the Cold and Flu
If you want a deep dive into an explanation of the biology of the common cold and flu (influenza) and how the immune system combats these infections, watch the video below presented by the world’s most favorite black-shirted neuroscientist, Dr. Andrew Huberman.
Click here for topic time stamps
00:00:00 Avoid Colds & Flu
00:01:58 Sponsors: Joovv, Helix Sleep & ROKA
00:06:00 Common Cold: Source & Transmission; Cold Temperature Myth
00:13:48 Spreading a Cold; Symptoms & Contagious Myths
00:17:43 Flu Virus & Transmission; Flu Shots
00:23:56 Tools: Injections & Safety; Charting Health Trends & Sickness
00:27:16 Sponsor: AG1
00:28:44 Spreading Cold & Flu, Symptoms
00:30:43 Immune System, Physical Barriers
00:39:33 Tool: Social Connection & Touch, Avoiding Flu & Cold
00:45:14 Innate Immune System
00:53:13 Sponsor: InsideTracker
00:54:15 Adaptive Immune System; Lymphatic System
01:00:19 Tools: Enhance Innate Immune System
01:06:19 Tool: Microbiome & Nasal Breathing
01:10:58 Tools: Enhance Gut Microbiome: Foods & Water Protocol
01:16:13 Exercise When Feeling Sick?, Sleep
01:21:39 Tool: Exercise & Preventing Sickness
01:28:13 Exercise When Sleep Deprived?
01:32:24 Tool: Exercise Recovery & Carbohydrates
01:34:52 Tool: Sauna & Enhance Immune System
01:42:20 Supplements: Vitamin C, Vitamin D
01:50:58 Echinacea, Zinc
01:55:08 N-acetylcysteine (NAC), Decongestants
The video dives into details about the immune system, explaining how it’s composed of the physical barrier (skin), the innate immune system, and the adaptive immune system. It clarifies that colds and flu are caused by viruses and there’s no cure for them.
The most effective prevention methods are avoiding contact with infected individuals and practicing good hygiene. And if you do catch a cold or flu, the video suggests ways to manage symptoms, such as getting plenty of rest, drinking fluids, and taking over-the-counter medications.
If you didn’t have two hours to spare, here’s my summary of the distinctions Dr. Huberman makes between viruses and bacteria, and colds and the flu.
Viruses vs. Bacteria
- Size: Viruses are much smaller than bacteria.
- Structure: Viruses are simpler in structure than bacteria. They lack the complex cell structures, such as DNA, ribosomes, and cell walls, that bacteria have.
- Reproduction: Viruses cannot reproduce on their own. They invade host cells and hijack their machinery to replicate. Bacteria can reproduce independently.
- Antibiotics: Antibiotics work against bacteria by targeting their cell walls or other essential structures. They have no effect on viruses.
Colds vs. Flu
- Cause: Colds are caused by rhinoviruses, while flus are caused by influenza viruses.
- Symptoms: Colds typically cause milder symptoms, such as runny or stuffy nose, sneezing, sore throat, and mild cough. Flus can cause more severe symptoms, such as fever, chills, muscle aches, headache, and fatigue.
- Duration: Colds usually last for a few days, while flus can last for a week or more.
- Treatment: There is no cure for either colds or flus, but there are treatments that can help manage the symptoms.
In the video, Dr. Huberman also discusses protocols related to behavioral tools and compounds that can help strengthen the immune system and potentially shorten the duration of colds or flu.
Here are the key protocols:
Behavioral Tools
- Sunlight exposure: Getting sunlight in your eyes as soon as possible after waking up helps set your circadian rhythm, daytime mood, focus, and alertness, and can improve sleep.
- Red light therapy: Using red light therapy devices like the Jujude handheld or panel can improve cellular and organ health, including faster muscle recovery, improved skin health, and wound healing.
- Sleep: Getting enough sleep is crucial for overall health, including immune function. The video recommends taking the Helix Sleep quiz to find a mattress that suits your sleep needs.
- Exercise: Regular exercise can help boost the immune system and improve overall health.
Compounds
- Vitamin D: Taking vitamin D supplements may help prevent colds and flu, although more research is needed.
- Zinc: Taking zinc lozenges within 24 hours of the first cold or flu symptoms may shorten the duration of the illness.
- N-acetylcysteine (NAC): Taking NAC may help shorten the duration of colds and flu, but more research is needed.
The Huberman video emphasizes that these protocols are not cures for colds or flu, and that some people may not benefit from them.
And now to the COVID-19 resurgence.
Why experts are concerned about the JN.1 variant responsible for latest COVID wave
The PBS Newshour video highlights the emergence of JN.1 as a potentially concerning COVID-19 variant, but emphasizes the need for further research and continued adherence to public health measures to mitigate the potential impact of this and future variants.
Here are the PBS Newshour’s key points:
Increased transmissibility: JN.1 appears to be even more transmissible than its predecessor BA.2, which itself was already highly contagious. This is attributed to mutations in the viral spike protein, making it easier for the virus to attach to and enter human cells.
Immune evasion: Experts are concerned that JN.1 might have some ability to evade existing immunity gained through vaccination or previous infection. This means it could potentially infect even vaccinated individuals and those who have already recovered from COVID-19.
Limited data: While initial data suggests some concerning characteristics, it’s still early days for JN.1. More research is needed to fully understand its potential impact, including its severity, hospitalization rates, and effectiveness of current vaccines against it.
Reasons for concern: The rise of JN.1 amidst declining levels of population immunity due to waning vaccine effectiveness and previous infections raises concerns about potential surges in cases and hospitalizations.
Recommendations: The video emphasizes the importance of:
- Staying up-to-date with vaccinations and boosters as recommended by health authorities.
- Considering masking in crowded indoor settings, especially those with vulnerable individuals.
- Maintaining good hygiene practices like handwashing and social distancing.
I haven’t done any of that since COVID has retreated from being the disruptive pandemic that upended our lives; hence, I got infected.
I’ve Got Covid-19: My Story
Six days ago I started to notice that something unwanted was knocking at my door. Unfortunately, I apparently didn’t have any choice in the matter — the door was knocked down and a series of symptoms ensued over the course of the last few days.
As mentioned previously, I’ve had a COVID vaccination and two boosters, the last one in February 2021. I didn’t get more recent boosters, such the one to (help) prevent JN.1 infection. I reasoned that if there’s a spike in COVID infections in Marin County, where I live just north of the Golden Gate Bridge, then I’d get the latest booster. Unfortunately, I wasn’t keeping tabs on what was going on, because there has been a spike here, as in many parts of the USA.
The Marin County Public Health Status Update stated:
“Winter respiratory virus season continues to accelerate in our community. For the past two weeks, more than one in ten visits to Marin County Emergency Departments have been due to respiratory virus symptoms. COVID-19 hospitalizations have risen 75% in the past week as the JN.1 variant spreads. Clinical testing and wastewater levels reveal the surge is due to a combination of flu, COVID-19, RSV and other viruses. Vaccination, and masking in crowded indoor settings, remains the most effective tools to stay healthy.”
U.S. COVID-19 Tracker Click here and enter your city and state for an update of the risk level in your community
Anyway, my inattentiveness has cost me a week of isolation and a bit of discomfort. I’m fortunate that I only experienced a sore throat for two consecutive mornings (it normalized in the afternoons), a drippy nose, a bit of phlegm and lethargy (I was, however, willing and able to walk two miles each day).
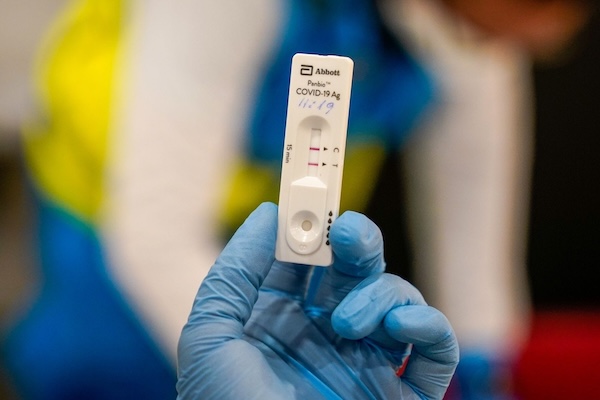
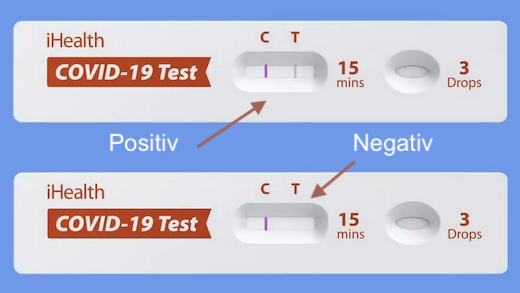
If it wasn’t for the at-home COVID tests I took, I would have thought I had a relatively mild case of the flu. This underscores the importance of testing.
I only had two expired test kits. The first one tested me negative, but given its expiry date was a year ago, I tested again, and the result was positive. OK, I thought, let’s try with a non-expired test, which my ever-stalwart sister provided. It confirmed the positive status.
Unfortunately, it’s common to be infectious before symptoms appear, and after they’re gone.
The window of infectivity for COVID-19 can vary, but generally falls within this range [1][2]:
- 2-3 days before symptoms: Research suggests viral shedding, and therefore potential infectivity, can begin 1-2 days before noticeable symptoms appear.
- 5-10 days after symptoms: Most people remain infectious for 5-10 days after symptom onset. In some cases, especially with individuals experiencing severe illness, this period may extend up to 20 days.
The CDC guidance suggests isolation for at least 5 days for mild to moderate cases and 10 days for moderate or severe cases, with continued mask-wearing for an additional 5 days for some individuals.
Today is my seventh day since symptoms were noted. I’ll test again in three days.
Order your free COVID-19 Tests via the USPS
COVID Vulnerability
Although I was grateful that my symptoms were mild, I’m mindful of the perils of so-called Long COVID, which I’ll address in a bit, but first let’s get our arms around what may be the root of COVID vulnerability — high baseline chronic inflammation.
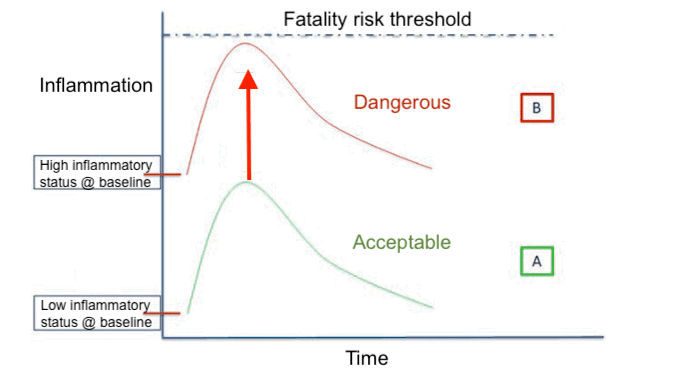
In the image above, scenario A depicts a spike in baseline inflammation due to an inflammation creating infection such as COVID-19. Because the baseline was otherwise low, this spike is within an acceptable range and is unlikely to create a hyperinflammtory response to the infection often referred to as a “cytokine storm”.
In scenario B, baseline inflammation is already high. This situation is typical among the populations that are vulnerable to adverse reactions to COVID-19 infection, such as the elderly, the obese and those with one or more of the indices that define metabolic syndrome. In this situation, a spike in an already high baseline inflammatory state can be dangerous.
The Link Between Chronic Inflammation and COVID Vulnerability
The hypothesis that high baseline chronic inflammation can increase susceptibility to COVID infection and lead to more severe symptoms is gaining traction, but it’s still an active area of research.
Let’s explore the potential mechanisms behind this connection:
1. Weakened Immune Response
Chronic inflammation can impair the immune system’s ability to fight off infections effectively. This can happen in several ways:
- Reduced immune cell function: Inflammatory mediators like cytokines can suppress the activity and proliferation of white blood cells, crucial for fighting viruses.
- Dysregulation of immune response: Chronic inflammation can lead to an overactive or imbalanced immune response, potentially causing damage to healthy tissues and hindering effective viral clearance.
- Impaired barrier function: Chronic inflammation in the lungs or respiratory tract can weaken the mucosal barrier, making it easier for viruses like SARS-CoV-2 to enter the body.
2. Cytokine Storm and Tissue Damage
COVID-19 can trigger a cytokine storm, an exaggerated immune response characterized by the release of large amounts of inflammatory molecules. In individuals with chronic inflammation, this storm can be further amplified, leading to:
- Increased lung damage: The inflammatory mediators can damage lung tissue, making it harder to breathe and potentially leading to acute respiratory distress syndrome (ARDS).
- Blood clotting and vascular problems: Chronic inflammation can contribute to blood clotting issues, which can worsen in severe COVID cases and lead to organ failure.
- Metabolic dysregulation: Chronic inflammation is linked to metabolic problems like insulin resistance and diabetes, which are also risk factors for severe COVID outcomes.
- Underlying Conditions and Comorbidities
Many chronic inflammatory conditions, such as obesity, diabetes, and autoimmune diseases, are also known risk factors for severe COVID-19. These conditions often share underlying mechanisms like chronic inflammation, oxidative stress, and endothelial dysfunction, which can all contribute to vulnerability to the virus.
Evidence Supporting the Link
While more research is needed to definitively establish causation, several studies suggest a link between chronic inflammation and COVID severity:
- A 2021 meta-analysis found that elevated baseline levels of inflammatory markers were associated with an increased risk of severe COVID-19 and mortality.
- A 2022 study reported that individuals with chronic inflammatory diseases like rheumatoid arthritis had a higher risk of hospitalization and death from COVID-19 compared to the general population.
- Research on long COVID suggests that chronic inflammation may play a role in the persistent symptoms experienced by some COVID patients.
Important Considerations
It’s important to remember that correlation doesn’t equal causation. While chronic inflammation may be associated with increased COVID vulnerability, it’s not the sole factor at play. Other individual risk factors like age, genetics, and underlying health conditions also contribute significantly.
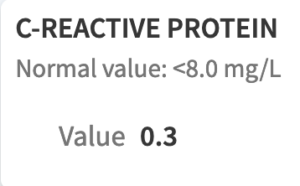
My hunch is that one of the reasons I’ve had mild COVID symptoms is due to my low baseline level of inflammation as indicated by two blood tests:
- C-reactive protein (CRP), and
- SED (sedimenation) rate.
Below is a screenshot of my lab results from a few months ago for each of these blood markers.
You can click on either image to get a bigger view.
Both of those values are quite low, and so, presumably, when I get a pro-inflammatory infection, the spike in inflammation is beginning at a low level and therefore doesn’t create a hyperinflammatory, cytokine storm-type reaction.
If your doctor does not test for these inflammatory blood markers, ask for them; otherwise, the Life Extension Foundation can accommodate you: CRP; SED rate.
Read How Dreaded Covid Inflammation Is Intensified by Age and Chronic Illness
And now let’s turn to long COVID
Long COVID: A Lingering Shadow of the Pandemic
Long COVID, also known as post-acute sequelae of COVID-19, is a complex condition that can affect individuals who have had COVID-19, even those with mild or asymptomatic initial infections. It’s characterized by a wide range of symptoms that can persist for weeks, months, or even years after the initial illness.
What is it?
The exact cause of Long COVID is still being researched, but it’s believed to involve a combination of factors, including:
- Persistent viral reservoirs: The virus may linger in certain tissues, even if it’s undetectable in standard tests.
- Autoimmune response: The body’s immune system may continue to attack itself, even after the virus is gone.
- Organ damage: The virus may directly damage organs, leading to long-term problems.
- Chronic inflammation: Long-term inflammation throughout the body may contribute to various symptoms.
Symptoms
The symptoms of Long COVID are diverse and can affect multiple body systems. Some of the most common include:
- Fatigue: This is the most common symptom of Long COVID, affecting up to 90% of patients.
- Brain fog: Difficulty concentrating, memory problems, and cognitive decline are frequently reported.
- Shortness of breath: This can be a debilitating symptom, making it difficult to exercise or even perform daily tasks.
- Muscle aches and joint pain: Widespread pain and aches are common, particularly in the muscles and joints.
- Sleep problems: Insomnia, difficulty falling asleep, and restless sleep are all common among Long COVID patients.
- Loss of taste or smell: While often associated with the initial COVID-19 infection, it can persist in Long COVID as well.
- Mental health issues: Anxiety, depression, and post-traumatic stress disorder (PTSD) are more common in people with Long COVID.
Prevalence
Estimates of the prevalence of Long COVID vary widely, but studies suggest that it affects 10-30% of people who have had COVID-19. This means millions of people worldwide are living with the long-term effects of the virus.
Long-term health issues
The long-term health consequences of Long COVID are still unclear, but research suggests it may increase the risk of developing other chronic conditions, such as:
- Cardiovascular disease: Heart problems, including heart failure and arrhythmias, are more common in people with Long COVID.
- Lung disease: Interstitial lung disease and chronic obstructive pulmonary disease (COPD) are potential complications.
- Kidney disease: Kidney dysfunction and even kidney failure have been reported in some cases.
- Neurological problems: Stroke, dementia, and epilepsy are some of the potential neurological complications.
Interventions
There is no one-size-fits-all cure for Long COVID, but there are various interventions that can help manage symptoms and improve quality of life. These include:
- Lifestyle changes: Getting enough sleep, eating a healthy diet, exercising regularly, and managing stress are crucial for overall health and well-being.
- Medications: Depending on the specific symptoms, medications like pain relievers, antidepressants, or sleep aids may be helpful.
- Rehabilitation: Physiotherapy, occupational therapy, and cognitive behavioral therapy can help manage fatigue, pain, and cognitive problems.
- Supportive care: Connecting with support groups and talking to a therapist can provide emotional support and help individuals cope with the challenges of Long COVID.
Living with Long COVID
Living with Long COVID can be challenging, both physically and emotionally. However, it’s important to remember that you’re not alone, and there are resources available to help you manage your symptoms and improve your quality of life. If you are experiencing any symptoms of Long COVID, it’s important to talk to your doctor to get a diagnosis and discuss treatment options.
Here are some additional resources that you may find helpful:
- The Long Covid Support Group
- The National Institute for Health and Care Excellence (NICE)
- The Centers for Disease Control and Prevention (CDC)
Science-backed Nutraceutical Support For Hyperinflammation
NLRP3 and Nuclear factor kappa (NF-κB) are key players in triggering and amplifying inflammatory responses. Their combined action can lead to hyperinflammation, a harmful excessive inflammatory state associated with various diseases, such as COVID-19.
First, I’ll briefly explain what are NLRP3 and Nuclear factor kappa (NF-κB), and then dig into eight nutraceuticals that can help.
NLRP3 and NF-κB
NLRP3 Inflammasome
- Sensing danger signals: NLRP3 acts as a sensor for diverse “danger signals” within the cell, including molecules released by damaged cells, pathogens, and metabolic imbalances.
- NLRP3 inflammasome assembly: Upon recognizing a danger signal, NLRP3 interacts with adaptor proteins and pro-caspase-1, forming the NLRP3 inflammasome complex.
- Caspase-1 activation: This complex activates caspase-1, a protease that cleaves pro-inflammatory cytokines interleukin (IL)-1β and IL-18 into their mature, active forms.
- Pyroptosis: NLRP3 activation can also trigger pyroptosis, a programmed cell death mechanism that contributes to tissue damage and inflammatory response amplification.
Nuclear factor kappa (NF-κB)
- Transcriptional activation: NF-κB is a transcription factor that regulates the expression of numerous genes involved in inflammation, such as pro-inflammatory cytokines, chemokines, and adhesion molecules.
- Positive feedback loop: NF-κB activation further stimulates NLRP3 expression, creating a positive feedback loop that intensifies the inflammatory response.
- Infiltration of immune cells: NF-κB promotes the recruitment and activation of immune cells like neutrophils and macrophages, leading to further tissue inflammation and potential damage.
Hyperinflammation
When NLRP3 and NF-κB are dysregulated or overactivated, their combined action can lead to hyperinflammation. This involves:
- Excessive production of pro-inflammatory cytokines: IL-1β and IL-18, along with other cytokines triggered by NF-κB, can cause widespread tissue damage and organ dysfunction.
- Recruitment and activation of immune cells: Increased immune cell infiltration can further amplify the inflammatory response and contribute to tissue destruction.
- Disruption of tissue homeostasis: The uncontrolled inflammatory response can disrupt normal tissue function and lead to organ failure in severe cases.
Click here for sources
- Inflammasome signaling: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6651423/
- Role of nlrp3 in hyperinflammation: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6651423/
- Nf-kb and nlrp3 interplay in chronic diseases: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6879348/
Eight Nutraceuticals that Can Help Reduce Hyperinflammation
Before I tell you about the eight nutraceuticals, I want to mention something that will help with prevention, a nasal spray called Xlear.
As I wrote in Can A Nasal Spray Kill Covid,
“…. a major preventive thing you can do for any viral respiratory illness is to irrigate your nasal passages with Xlear nasal spray at the end of every day, and after any exposure to crowds (work, school, playgroups, plane travel, etc.)”.
I further wrote about Dr. Frances Lund’s perspective about “local immunity”. She’s a University of Alabama at Birmingham immunologist working with biotech Altimmune Inc. on an early-stage nasal inoculation, and says that local immunity matters.
Says Dr Lund:
“The vaccines that can be delivered to generate that will have some advantages over vaccines that are delivered systemically… You still get systemic immunity if you deliver it via the intranasal route, so that doesn’t go away, and you add a level of immunity that you don’t get with an intramuscular vaccine. And that immunity is local.”
You typically get COVID by touching something infected with it and then touching your eyes, and the virus enters the body there, or by being close enough to an infected person who sneezes, coughs or otherwise expels the virus into some invisible cloud that gets into your respiratory tract.
I’m not saying that Xlear is some magical solution, just that there’s some evidence it could be helpful [3][4][5], along with, of course, washing your hands frequently and wearing a mask when in enclosed spaces with numerous people milling around.
Now to the nutraceuticals…
Research studies support the following eight nutraceuticals to potentially be helpful to prevent or reduce the hyperinflammation caused by NLRP3 and Nuclear factor kappa ?:
- Potassium
- Curcumin
- Bromelain
- Resveratrol
- Quercetin
- Boswellia
- Sulforaphane
- PEA
Let’s examine each nutraceutical in terms of its potential to tamp down hyperinflammation.
Potassium
Potassium is one of seven essential macrominerals. The human body requires at least 100 milligrams of potassium daily to support key biological processes, although that is the bare minimum, not a healthy amount.
Maintaining blood potassium levels is important to prevent potassium cellular efflux, which is a condition where the potassium content of cells flow out of them.
Potassium cellular efflux upregulates inflammasome assembly, which is a fancy way of saying that insufficient potassium in cells are responsible for the activation of inflammatory responses.
Because potassium is easily obtained from foods, such as apricots, beans, squash and potatoes, deficiencies in the macromineral are uncommon unless you:
- Use certain medicines, such as diuretics.
- Have physically demanding jobs.
- Athletes exercising in hot climates and sweating excessively.
- Have health conditions that affect their digestive absorption, such as Crohn’s disease.
- Have an eating disorder.
- Smoke.
- Abuse alcohol or drugs.
Curcumin
Curcumin is a compound in turmeric, the common Indian spice. It has well-documented beneficial health effects, such as antiviral and anti-inflammatory activity.
It’s also been shown to suppress NLRP3 activation, and is thought to have the potential to halt viral entry into host cells.
Although you can get curcumin from eating the Indian spice turmeric, it’s highly unlikely you’ll get sufficient quantities to have a therapeutic effect, especially given that curcumin is poorly absorbed. Your best bet is to supplement with a curcumin formulation that enhances bioavailability. Check the Nutraceutical Guide for recommendations.
Bromelain
Bromelain is an enzyme extract derived from the stems of pineapples. Many studies have documented the ability of bromelain to reduce inflammation and inflammatory diseases.
Of particular importance here is bromelain’s documented ability to decrease tissue edema and inflammation. Several studies have shown that bromelain is effective in respiratory conditions such as asthma, bronchitis, and sinusitis that are characterized by increased mucus production and inflammation.
Research also shows that bromelain decreases cytokines. A placebo-controlled randomized clinical trial found that high-dose oral bromelain showed immunomodulation of both Th-1 and Th-2 cytokines.
Resveratrol
Resveratrol is a natural chemical (a stilbenoid) produced by several plants in response to injury or when the plant is under attack by pathogens. Sources of resveratrol in food include the skin of grapes, blueberries, raspberries, peanuts and coca.
Resveratrol has been shown to reduce inflammation, as well as to inhibit the mitochondrial damage in macrophages, which can happen when the NLRP3 inflammasome is initiated.
If you choose to supplement with resveratrol, choose the trans resveratrol formulation. As I wrote in a post about trans-resveratrol:
“Trans-resveratrol is the best resveratrol supplement you can take simply because your body can absorb it better. Regular resveratrol is not very bioavailable, thus compromising its potential health benefits.”
Boswellia
Boswellia, also called Indian frankincense, is a resin herbal extract from the boswellia tree that exerts a number of anti-inflammatory effects. It’s been shown to significantly inhibit NFKB signaling, although I should point out that these were in mice models.
Nonetheless, boswellia is on our list of inflammatory-suppressing nutraceuticals, because even though you’re not a mouse, boswellia has been used for centuries to treat chronic inflammatory illnesses. Moreover, a July 2020 study not yet peered reviewed found that:
“Out of eleven compounds, β-boswellic acid (Boswellia serrata) was found to be best suitable along with Glycyrrhizic acid (Glycyrrhiza glabra). Being medicinal compounds, their efficacy was found to be higher than conventionally available anti-viral, anti-inflammatory and anti-malarial drugs. With the advantage of being natural source, it features no harmful side effects, these novel compounds make a great choice to be used for the treatment of COVID patients.”
As you may recall from Lesson 13, Glycyrrhiza glabra is Licorice root. Combining it with boswellia appears to be a potent combination against the potentially unregulated inflammatory reaction of the immune system to viral infection.
EGCG
EGCG (epigallocatechin gallate) is a polyphenol with potent health protective effects against several chronic diseases, but here our focus is to tamp down the immune system’s potential lingering and accelerating inflammatory response to Covid. To that end, EGCG can help modulate the NLRP3 inflammasome, potentially targeting the SARS-CoV-2 main protease (a type of protein) to reduce viral replication, and has also been shown to prevent influenza in healthcare workers.
You can supplement with an EGCG extract, but getting it from high-EGCG content tea may be a better, more natural source. Brewed tea contains the highest concentration of EGCG, and its concentration increases with brewing time. To maximize EGCG content, pour boiling water (not just hot water) over a green tea bag, and let steep for ten minutes before drinking it.
EGCG, like other catechins, binds to proteins in our food and make them less absorbable into your bloodstream; thus, drink the tea between meals rather than directly with food to get the most benefit. EGCG can also bind with minerals in food such as iron; this also reduces its absorption, and provides an additional reason to consume green tea separately from other foods.
Sulforaphane
Sulforaphane is a well-studied anti-inflammatory phytochemical found in cruciferous vegetables, such as broccoli (especially the sprouts), cabbage, cauliflower, Brussels sprouts, Swiss chard and bok choy.
Sulforaphane inhibits NLRP3 inflammasome biology. It also activates an antioxidant pathway [Nrf2] pathway and upregulates glutathione levels.
What that translates to is that sulforaphane helps to tamp down excess inflammation, while improving the ability of our body to produce more of its “Master Antioxidant”, glutathione.
It’s noteworthy that curcumin, resveratrol, quercetin, and berberine have all been shown to promote AMPK (adenosine 5′ monophosphate-activated protein kinase).
AMPK is an enzyme that plays a role in cellular energy homeostasis, largely to activate glucose and fatty acid uptake and oxidation when cellular energy is low. It’s also a promoter of SIRT2 (one of seven sirtuin genes in mammals involved in ageing, energy production and lifespan extension) that is known to inhibit NLRP3 inflammasome assembly.
PEA
PEA (Palmitoylethanolamide) is a naturally occurring food component that is an anti-inflammatory palmitic acid derivative that interfaces with the endocannabinoid system.
(Palmitic acid is the most common saturated fatty acid found in animals, plants and microorganisms. The endocannabinoid system is one composed of endogenous lipid-based neurotransmitters that bind to cannabinoid receptors and cannabinoid receptor proteins that are expressed throughout the vertebrate central nervous system.)
PEA has emerged as a useful nutraceutical, because this compound is naturally produced in many plant and animal food sources, as well as in cells and tissues of mammals, and is endowed with important neuroprotective, anti‐inflammatory and analgesic actions.
A 2013 study published in the International Journal of Inflammation found a significantly favorable outcome in five of six double blind placebo-controlled trials looking at acute respiratory disease due to influenza.
There are multiple mechanisms of action associated with PEA that result in attenuating the potentially fatal cytokine storm, as well as being an effective agent in relieving inflammatory and neuropathic pain.
If you have the misfortune of getting into this hyperinflammatory phase, consider taking the nutraceuticals I just reviewed. That said, at this point hopefully you’ll also be under your doctor’s care.
Last Updated on January 20, 2024 by Joe Garma