Why Your LDL Cholesterol Particle Size Determines Your Heart Disease Risk and What To Do About It
If you have high cholesterol, you must know your LDL cholesterol particle size! It’s the key determinant of your chances of dying from heart disease, the worst chronic health disease and the number one killer. Here’s what it is, how to test for and reduce it.
GIVEN THAT you have a significant chance to developing the most prevalent chronic condition as you get older that is the #1 killer in America and many industrialized nations, wouldn’t you want to know how to prevent it?
Or, given that you have a significant chance to already have this condition, wouldn’t you want to know how to pulverize it?
Than grab your scuba gear, because we’re about to do a deep dive on the topic of cholesterol and heart disease. Specifically, I’m going to reveal why your doctor is probably NOT testing you for the type of cholesterol that does the most damage and is the verifiable risk factor for heart disease.
Once you’ve read this article, please share it widely, because you do have friends and family who need to know whether they really know if their cholesterol diagnosis is relevant and what to do about it.
WARNING!
Did I mention that this is a “deep dive”? You may need to come up for air, take a siesta, before you dive back in, but I encourage to at least get a sense for the material here presented. Perhaps watch some video. If you ever get diagnosed as being at high risk for heart disease, you’ll want come back and get your feet wet.
In this article, you’ll discover:
- Sobering cholesterol stats brought to you by the World Health Organization.
- Demystifying which cholesterol we need and which is harmful.
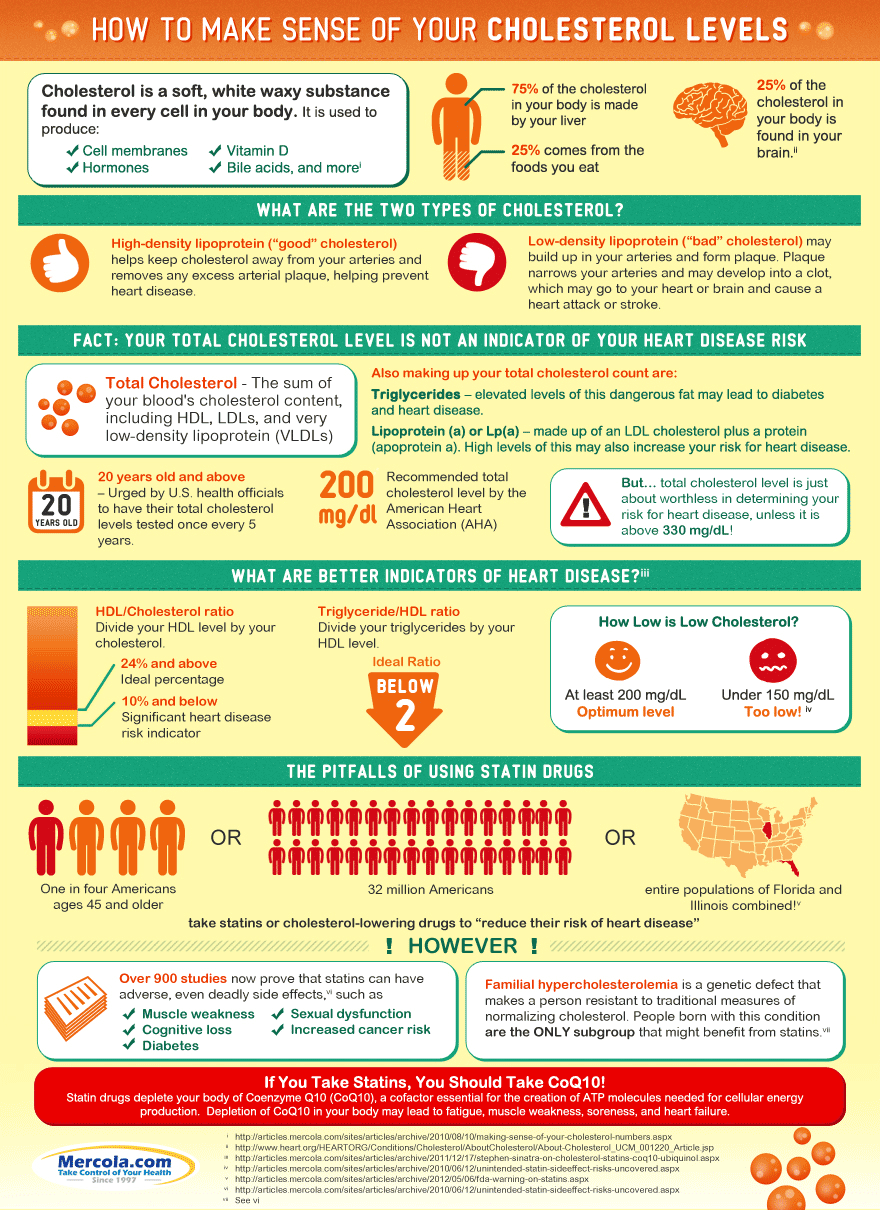
- An infographic by Dr. Mercola that explains what is and isn’t cholesterol.
- How inflammation weaponizes cholesterol.
- The Functional Medical approach to analyzing and treating high cholesterol, particularly LDL cholesterol particle size.
- An online test you can take. (I did and show my results.)
- Four short videos by the brilliant Dr. Greger that prove LDL is the culprit and what you can do about it.
Let’s dive in…
Sobering Statistics From the WHO
No, not the band, but the World Health Organization reports that in 2008 the global prevalence of raised total cholesterol among adults was 39% (37% for males and 40% for females). (1) In the U.S., the CDC reports that more than 102 million American adults (20 years or older) have total cholesterol levels at or above 200 mg/dL, which is commonly thought to be above healthy levels. More than 35 million of these people have levels of 240 mg/dL or higher, putting them at high risk for heart disease. (2)
As you’ll soon see, there’s quite a debate about what level of total cholesterol is tolerated by our body, but what stands as gospel is that the main culprit behind heart disease, the number one killer worldwide, is LDL, the so-called “bad cholesterol”.
Back to some CDC stats (3):
- 73.5 million adults (31.7%) in the United States have high low-density lipoprotein (LDL), or “bad,” cholesterol.
- Fewer than 1 out of every 3 adults (29.5%) with high LDL cholesterol has the condition under control.
- Less than half (48.1%) of adults with high LDL cholesterol are getting treatment to lower their levels.
- People with high total cholesterol have approximately twice the risk for heart disease as people with ideal levels.
The focus of this article is to convince you to get tested for a particular form of LDL, which if too high can strongly contribute to all sorts of heart disease.
Let’s begin with Dr. Joseph Mercola.
Dr. Mercola: Let’s Demystify Cholesterol — Know Your LDL cholesterol Particle Size Particulars
Famed online health guru Dr. Joseph Mercola wrote an informative article entitled, “The Cholesterol Myth“, wherein he makes the following points:
- Your body needs a certain amount of cholesterol.
- You need to know the type of cholesterol that’s harmful.
- Inflammation weaponizes cholesterol.
The rest of this section is guided by Dr Mercola’s article.
Your Body Needs It and Makes It
Cholesterol is a “soft, waxy substance is found not only in your bloodstream, but also in every cell in your body, where it helps to produce cell membranes, hormones, vitamin D and bile acids that help you to digest fat”. (4)
It exists in your body for two reasons: your liver makes it (about 75%) and you ingest it (primarily from saturated fat sources, like diary and meat food products).
The two basic types of cholesterol are:
- High-density lipoprotein or HDL: This is the “good” cholesterol that helps keep cholesterol away from your arteries and remove any excess from arterial plaque, which may help to prevent heart disease.
- Low-density lipoprotein or LDL: This “bad” cholesterol circulates in your blood and, according to conventional thinking, may build up in your arteries, forming plaque that makes your arteries narrow and less flexible (a condition called atherosclerosis). If a clot forms in one of these narrowed arteries leading to your heart or brain, a heart attack or stroke may result.
In addition to HDL and LDL, a type of fat and a fat-transporting protein are a part of your total cholesterol count:
- Triglycerides are a dangerous type of fat because elevated levels are linked to heart disease and diabetes. Triglyceride levels are known to rise from eating too many grains and sugars, being physically inactive, smoking cigarettes, drinking alcohol excessively and being overweight or obese.
- Lipoprotein (a), or Lp(a), is a substance comprised of LDL plus a protein (apoprotein a). Elevated Lp(a) levels are a very strong risk factor for heart disease. This is an important measure of LDL cholesterol particle size, which has been well established, yet very few physicians test their patients for it.
The Harmful Part of Cholesterol Are the LDL Particles
Dr. Mercola highlights the work of Ron Rosedale, MD, widely considered to be the leading anti-aging doctor in the United States, who explains the differences between harmful and benign cholesterol: (5)
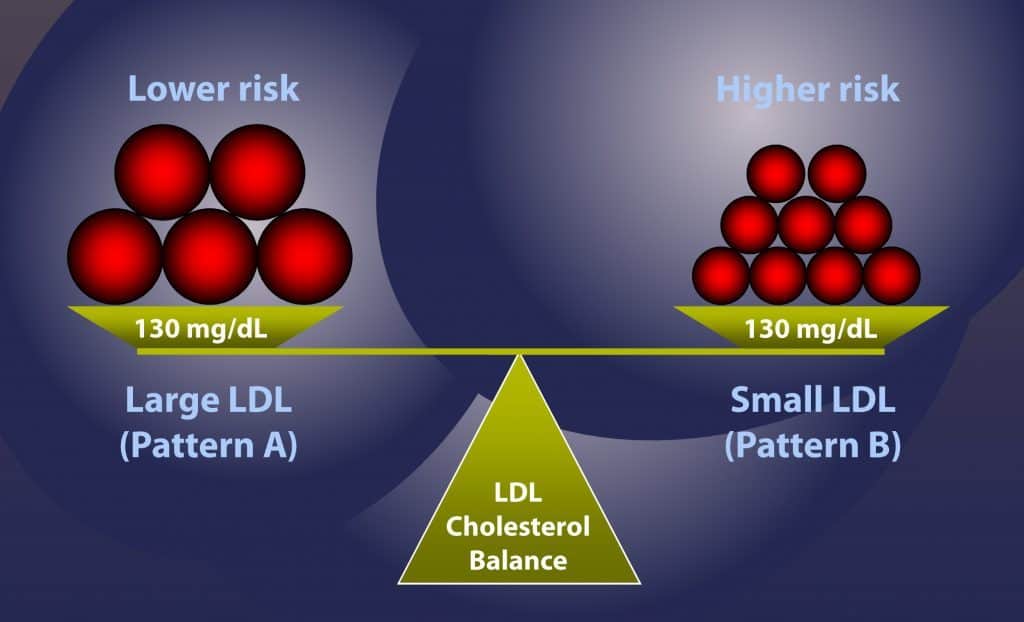
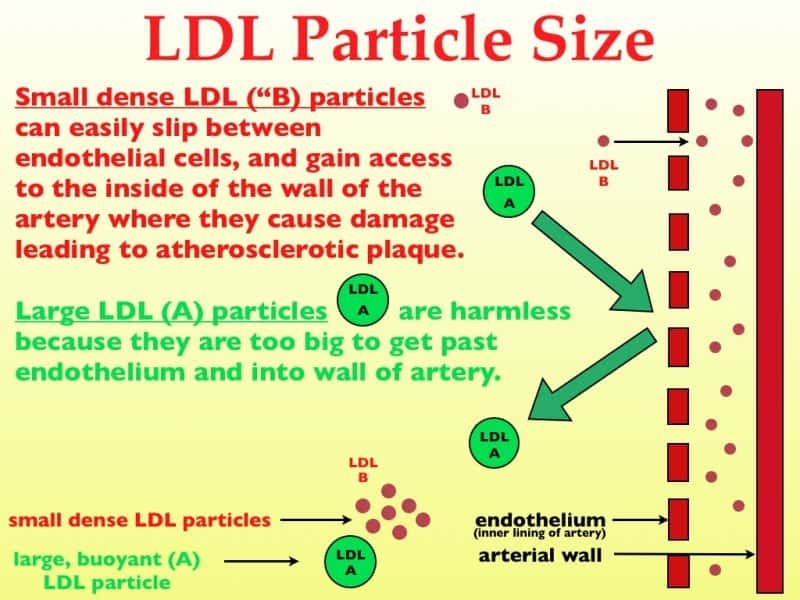
“Notice please that LDL and HDL are lipoproteins — fats combined with proteins. There is only one cholesterol. There is no such thing as ‘good’ or ‘bad’ cholesterol. Cholesterol is just cholesterol. It combines with other fats and proteins to be carried through the bloodstream, since fat and our watery blood do not mix very well. Fatty substances therefore must be shuttled to and from our tissues and cells using proteins. LDL and HDL are forms of proteins and are far from being just cholesterol.
In fact we now know there are many types of these fat and protein particles. LDL particles come in many sizes and large LDL particles are not a problem. Only the so-called small dense LDL particles can potentially be a problem, because they can squeeze through the lining of the arteries and if they oxidize, otherwise known as turning rancid, they can cause damage and inflammation.
Thus, you might say that there is ‘good LDL’ and ‘bad LDL.’ Also, some HDL particles are better than others. Knowing just your total cholesterol tells you very little. Even knowing your LDL and HDL levels will not tell you very much.”
As Dr. Rosedale said above, the main cholesterol-based culprit in heart disease are LDL particles, which include one called lipoprotein(a), again, a common LDL cholesterol particle size and type.
When you get your cholesterol checked, ask your doctor to use a “VAP” test, or one similar.
As the Life Extension Foundation puts it:
“The VAP test assesses levels of all the blood lipids measured in a standard lipid profile (total cholesterol, LDL, HDL, and triglycerides), plus subclasses of lipids that are known or emerging risk factors for cardiovascular disease, such as LDL particle size and lipoprotein(a)” (6)
Click here to see my VAP test results.
“VAP” stands for “Vertical Auto Profile” (don’t ask), and it tests for more cholesterol particles, and at a more refined level, than standard tests, such as these:
- A more accurate, direct measurement of LDL.
- Measurement of LDL pattern density, important because small, dense LDL (“Pattern B”) triples the likelihood of developing coronary plaque and suffering a heart attack.
- Measurement of lipoprotein subclasses, which include HDL2 and HDL3, intermediate-density lipoprotein (IDL), very-low-density lipoproteins (VLDL1, VLDL2, VLDL3), and other lipoproteins that can lead to heart attacks and strokes.
Here are a few of the VAP Cholesterol results of my 2013 LEF blood panel:
| Test | Result/Unit | Reference Interval |
| Cholesterol, Total | 167 mg/dl | Less 200 |
| HDL Cholesterol | 53 mg/dl | Above 40 |
| LDL Cholesterol | 97 mg/dl | Less 130 |
| Total/HDL Ratio | 3.2 | 0-5 |
| VLDL | 17 mg/dl | Less 30 |
| HDL -2 (most protective) | 9 mg/dl | Greater 10 |
| VLDL-3 (small remnant) | 10 mg/dl | Less 10 |
| LDL Density Pattern | B | Abnormal |
Yes, everything was looking rosy as long as the 2013 test measured what it did in 2012, but thanks to the details of the VAP test, I discovered that I might have some issues; namely:
- HDL-2, at 9 mg/dl is too low, which could indicate susceptibility to coronary artery disease.
- VLDL-3, at 10 mg/dl, is too high and could indicate susceptibility to type-2 (adult-onset) diabetes, which my father and uncle had.
- A LDL Density Pattern of “B” means the LDL cholesterol “balls” are small and dense, which could rupture arterial walls (think those air gun BBs), rather than the “fluffy” Patter “A” LDL, which is far less damaging.
Read more about this in my article, Four Tests That Will Tell You The Truth About Your Health.
Note: I got my VAP test via the Life Extension Foundation, but they don’t appear to offer it anymore, but do have a more extensive test called, NMR-LipoProfile-PLUS.
Given that the LDL cholesterol particle size causes the damage, “total cholesterol” is a useless cholesterol measurement, insists Mercola. He points out that the American Heart Association recommends that total cholesterol should be less than 200 mg/dL, but that this total cholesterol level is a poor determinant of your risk for heart disease, unless it’s above 300 mg/dL.
Moreover, he asserts, to achieve the very low American Heart Association 2004 recommended guidelines of below 100 mg/dL, or 70 mg/dL for patients at very high risk, practically ensures that you will need to take cholesterol-lowering drugs.
In his clinic, Dr. Mercola has seen people with total cholesterol levels over 250 mg/dL who were at low heart disease risk due to their high HDL levels, and in contrast, has seen those with cholesterol levels under 200 that were at a very high risk of heart disease based on the following additional tests:
- HDL/Cholesterol ratio (above 24% is good)
- Triglyceride/HDL ratio (below 2 is good)
HDL percentage is a very potent heart disease risk factor. Just divide your HDL level by your cholesterol. That ratio should ideally be above 24%. You can also do the same thing with your triglycerides and HDL ratio. That ratio should be below 2.
But, as I wrote earlier, these markers do not provide a complete picture of your cholesterol profile, nor do they indicate if you’re at risk for developing heart disease.
This is why I want to tell you about VLDL through the lens of Chris Kresser, but first check out Dr. Mercola’s cholesterol infographic below to summarize what you’ve learned, followed by some important insights about how chronic inflammation weaponizes LDL.
Inflammation Weaponizes Cholesterol
Before we leave Dr. Mercola’s views on cholesterol (and get into Chris Kresser’s and Dr. Micheal Greger’s perspectives on the subject), it’s very important to glean what he has to say about the role inflammation has to, in effect, weaponize cholesterol by making it’s potential impact on heart disease very damaging.
Chronic inflammation is now widely considered to be either an important part of what causes or amplifies the effects of chronic diseases, and even aging.
Inflammation is your body’s vitally important, protective response to harmful invaders, such as pathogens, damaged cells, or irritants. For instance, if your skin gets cut, the process of inflammation enables you to heal by:
- Constricting blood vessels to keep you from bleeding to death.
- Thickening the so it can clot.
- Actively participating in with your immune system that “sends” cells and chemicals to fight viruses, bacteria and various pathogens that could infect the area.
- Supports cellular division to repair the damage.
In this instance, the inflammation stick around only as long as it’s role in the healing process is over; however, in the case of “chronic inflammation”, the healing never happens and the biological cascade of inflammation is never shut off.
Chronic inflammation is what enables cholesterol — specifically LDL cholesterol particle size — to damage arteries. This happens similarly to our skin cut example, except that the “scar” in your artery is known as plaque.
This plaque — along with the thickening of your blood and constricting of your blood vessels that normally occur during the inflammatory process — can increase your risk of high blood pressure and heart attacks before cholesterol enters the picture.
In this instance, cholesterol becomes involved as it’s necessary to replace the cells damaged by plaque and cells require cholesterol to form. When damaged cells need replacing, the liver makes cholesterol. If the inflammation is chronic, the liver will be making and releasing cholesterol into the bloodstream regularly.
The test usually used to determine if you have chronic inflammation is a C-reactive protein (CRP) blood test. CRP level is used as a marker of inflammation in your arteries:
- A CRP level under 1 milligrams per liter of blood means you have a low risk for cardiovascular disease.
- 1 to 3 milligrams means your risk is intermediate.
- More than 3 milligrams is high risk.
(Read: 8 Risk Factors for Chronic Inflammation and What To Do About It)
Now, let’s let Chris Kresser wade into the LDL cholesterol waters with us.
Chris Kressers’ Functional Medical Perspective On Cholesterol
Along with Joseph Mercola, Chris Kresser — a functional medicine expert and acupuncturist — has long challenged the established medical orthodoxy that “cholesterol is bad and if you have high cholesterol you should take a statin to lower it.”
He says that this claim is outdated and doesn’t reflect recent scientific evidence, and that such findings have yet to reorient the views of the average primary care doctor, or cardiologist.
You’ll find many of the details of his perspective on cholesterol similar to Dr. Mercola’s.
In a recent interview, Kresser tackled these main points about the insufficiency of typical cholesterol tests to determine if your at risk for heart disease:
- High cholesterol is in itself not a disease but a symptom of six primary underlying causes, which if properly addressed can often alleviate the need to take statins.
- Conventional lipid markers are not accurate, nor sufficient predictors of cardiovascular risk associated with heart disease.
- Recommended tests to assess your risks of heart disease.
- How his clinical practice addresses patients with very high LDL cholesterol particle size.
The Six Primary Causes of High LDL
As a clinician and researcher, Chris Kresser has come to rely on these six primary causes of high LDL:
- Metabolic dysfunction.
- Chronic infections like H. pylori or latent viral infections.
- Gut dysbiosis permeability.
- Poor thyroid function, whether it’s full-on hypothyroidism, subclinical hypothyroidism (doesn’t present clear symptoms) or the thyroid is under-functioning.
- Environmental toxins, especially heavy metals.
- Genetic.
His functional medicine approach is to explore all of these root causes to determine and address their specific pathology, because if you treat the root, that will often fix the branches — the symptoms. He explains that if you think of the disease process like a tree, the roots are those core pathologies or underlying mechanisms that lead to the symptoms; in this analogy, the branches.
The conventional medical approach is to get tangled in the branches and try to deal with things on that level, but by doing so, the root of the problem is not uprooted.
In the conventional paradigm, the focus is on symptom suppression. If you have high cholesterol, you take a drug to lower it, a statin. If you have high blood pressure, or high blood sugar, drugs are the prescribed solution, as they are for many other chronic health conditions.
Why Lipid Markers Are Inaccurate and Insufficient Cardiovascular Risk Predictors
Lipid markers that are routinely tested are total cholesterol, HDL cholesterol and LDL cholesterol, which is as you know by now is the so-called “bad cholesterol”. When you go to your doctor for a blood workup, that’s what’s tested and that’s a problem because they’re not accurate predictors of cardiovascular risk, says Kresser.
Like Dr. Mercola, Kresser says the ratio of total-to-HDL cholesterol as well as non-HDL cholesterol are better predictors than total cholesterol, but Kresser insists that they are nowhere near as predictive for heart disease as some of the newer markers like LDL cholesterol particle size and number, including lipoprotein(a), or Lp(a), a component of LDL cholesterol. These markers, they tell us something different than the standard lipid markers.
The standard lipid markers tell us how much cholesterol is inside of the lipoproteins, so if we use Kresser’s analogy that your bloodstream as like a highway, the passengers inside of a car are equivalent to cholesterol inside the lipoproteins, whereas the cars themselves would be equivalent to the lipoproteins themselves.
Extending this analogy, if you have lots of cars on the road, there’s a much greater chance for accidents to occur. These cars will slam into the side of the road; in this analogy, into the fragile lining of the artery, the endothelium.
If you have a lot of LDL particles, which is reflected in the LDL particle number measurement, there’s a much greater likelihood that one of these LDL particles is going to damage the fragile endothelium and initiate the process of plaque formation.
Kresser asserts that of all of the things we could measure in terms of lipid markers, lipoprotein(a), or Lp(a) — one measure of LDL cholesterol particle size — is the most predictive for future risk of heart disease.
Inflammation, Insulin and Other Important Cardiovascular Risk Markers
One thing you can say about Chris Kresser is that he’s thorough.
When it comes to assessing the overall risk for heart disease, he wants to look at a hose of risk markers, such as:
- Inflammation markers
- C-reactive protein,
- Fibrinogen
- Lp-PLA2
- Oxidized LDL
- Metabolic markers
- Fasting insulin
- Fasting glucose
- Fasting leptin
- Post-meal blood sugar
- Hemoglobin A1c
- Hypertension
- Smoking
- Diet
- Vitamin D
- Iron
- Gut microbiota
Test Your Heart Disease Risk Exposure — I Did
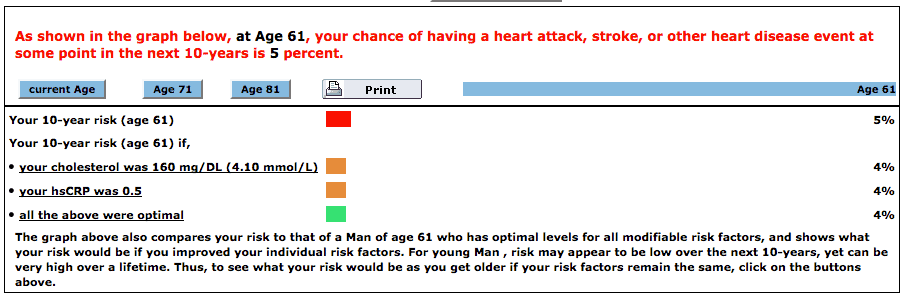
Kresser points out that there exist online assessments that use some of the aforementioned risk factors to provide a probability of getting heart disease. The Reynolds Risk Score, for example, uses C-reactive protein and systolic blood pressure in addition to age, total cholesterol, HDL cholesterol, and family history to determine the 10-year risk of heart disease expressed as a percentage.
I just took it, and this is a screen shot of my results (click pic to enlarge):
Note from the test results above that if my c-reactive protein number (a measurement for inflammation) was lower (0.5) rather than 3.7 mg/L (which is high), my 10 years risk of having a heart attack would drop to 4%, rather than 5%.
There are other types of testing that look for objective evidence of plaque accumulation, like a calcium score and CIMT, and these are tests that a doctor can do when/if they are warranted, and they provide a different angle. The lipid markers are just looking at blood markers that are typically associated with heart disease, but a calcium score and carotid intima-media thickness test can tell you what’s actually happening in terms of plaque accumulation.
How Kresser Treats Patients with Familial Hypercholesterolemia
Familial Hypercholesterolemia (“FH”) is is a genetic disorder characterized by high cholesterol levels, specifically very high levels of low-density lipoprotein (LDL, “bad cholesterol”), in the blood and early cardiovascular disease.
If you can treat this successfully, it’s likely that reducing the garden variety high LDL is a cake walk. I’ll summarize Kresser’s approach to treating Familial Hypercholestreolemia, but suggest you click over to his article and read the details if interested.
Here’s how Kresser treats FH:
- Test to determine LDL particle number, lipoprotein(a), and other important markers are like—fasting insulin, fasting post-meal glucose, inflammatory markers etc.
- Do a thorough medical and family history.
- Determine likelihood of contributing factors like SIBO, dysbiosis, infections, heavy metal toxicity, hypothyroidism, etc.
- Get a lifestyle assessment relative to diet and stress.
- Potentially, get a calcium score (CIMT).
If patients are a hyper-responder to saturated fat that increases their LDL particle number, Kresser might put them on what he refers to a “Mediterranean Paleo” diet, which is Paleo that’s lower in fat and higher in Paleo-friendly carbohydrates, whole-food carbohydrates like starchy plants, whole fruits, non-starchy vegetables, with an emphasis on monounsaturated fat as opposed to saturated fat.
Additionally, he might use some supplements that have been shown to reduce LDL particle number and address inflammatory processes like delta and tocotrienols, pantethine, curcumin, etc., and these will often lead to a significant reduction in these various biomarkers that are risk factors for heart disease, even lipoprotein(a), which is in the conventional paradigm, thought to be almost entirely genetically mediated and not really amenable to diet and lifestyle change.
Click here to listen to Chris Kresser talk about the functional medicine approach to high cholesterol.
Finally, we get to Dr. Michael Greger, a medical doctor, a leading expert in nutrition and Founder and chief contributor to a fantastic fact-based website called Nutrition.org.
Dr. Greger On Why LDL Causes Heart Disease and What To Do About It
By now those few of you who made it here have weary eyes from all that reading, so we’re going to turn to Dr. Michael Greger for some video depictions of studies and graphic presentations of all that cholesterol stuff you’ve read about above.
Here’s what we’re going to cover in this section, courtesy of Dr. Greger:
- The optimal LDL level;
- Why oxidized LDL triggers inflammation; and
- Two foods to eat to knock down high LDL.
Note that Dr. Greger doesn’t specifically use the term “LDL cholesterol particle size”. I think this is for the same reasons that many experts in this field do not — it gets complicated — and so they believe it’s sufficient call all the components of LDL as simply “LDL” without pointing out the specifics and relative differences.
That fine, but remember that when you get your cholesterol tested, you want to ensure you get our LDL cholesterol particle size tested using a VAP test, as described above, or some similar test.
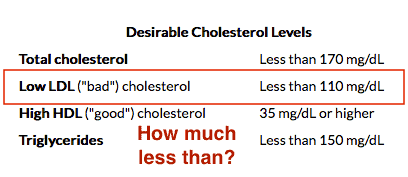
These are the typical cholesterol numbers deemed desirable by most health practitioners:
Lots of “less than” is desired, but how much less than?
In his “optimal cholesterol video“, Dr. Greger gets right to it:
“The optimal cholesterol level, the optimal “bad cholesterol” LDL level, is 50 to 70″
He says that data from multiple lines of evidence consistently demonstrate that between 50 and 70 mg/dL is where the physiologically normal LDL level would be. Above this threshold above is where atherosclerosis and heart attacks develop.
Where did Dr. Greger get that LDL range?
Turns out, that’s what we start out with at birth, that’s what our fellow primates have and that’s the level seen in populations free of the heart disease epidemic. Moreover, we can look at all the large randomized controlled cholesterol-lowering trials that show the same thing.
In his video below, Dr. Greger reviews various studies that show the progression of atherosclerosis versus LDL cholesterol. The more cholesterol, the more atherosclerosis. The place where you can estimate the LDL level at which there is zero progression is at a LDL cholesterol of 70 mg/dL.
You can do the same with the studies preventing heart attacks. Zero coronary heart disease events might be reached down around 55 md/dL, and those who’ve already had a heart attack and are trying to prevent a second one might need to push their LDL levels even lower.
Optimal LDL Cholesterol Level
You may find the original video and transcript here.
Atherosclerosis is endemic in much of the world’s industrialized populations in part because the average person’s LDL level is up around 130 mg/dL, approximately twice the normal, untainted physiologic level.
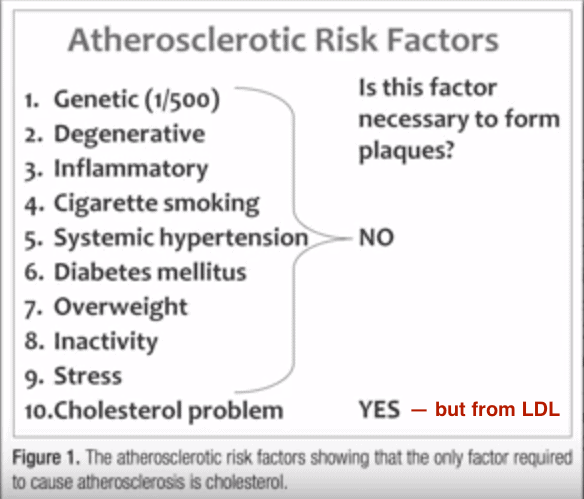
No other atherosclerotic risk factor results in plaque buildup:
The U.S. federal government doesn’t recommend that everyone try to reduce LDL to just under 100 mg/dL, Dr. Greger claims, is because — despite the lower risk accompanying more optimal cholesterol levels — the intensity of clinical intervention required to achieve such levels for everyone in the population would financially overload the health care system. Drug usage would rise enormously.
But they’re assuming drugs are the only way to get our LDL that low, whereas eating really plant-based diets may hit the optimal cholesterol target without even trying.
Why Oxidized LDL Triggers An Inflammation Response
When LDL infiltrates the lining of our artery it gets oxidized, and triggers an inflammatory response. When this happens, the lining of your artery produces adhesion molecules to stick white blood cells, called monocytes, which try to repair some of the havoc the cholesterol is wreaking.
Simply put: we never evolved to have so much cholesterol in our bloodstream, and it causes damage and inflammation inside the walls of our arteries.
Arterial Acne
You may find the original video and transcript here.
Two foods to eat to knock down high LDL
Now that Dr. Greger has confirmed that which by now you already knew — that LDL is the cholesterol culprit behind heart disease — how about getting his perspective on two simple ways to lower it; namely:
- Eat nuts; and
- Eat phytosterol-rich foods.
Surely, you know about nuts, so let’s look at the phytosterol-rich foods first. Phytosterols are a family of molecules related to cholesterol found in the cell membranes of plants, where they play important roles, just as cholesterol for us.
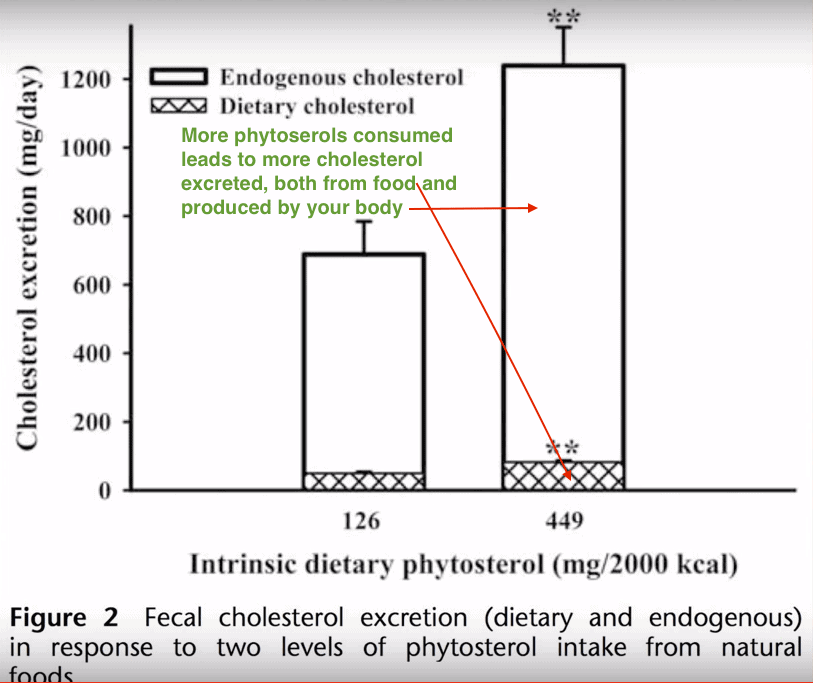
In the next video, Dr, Greger reports that when we eat phytosterol-rich foods like green veggies, nuts and seeds, the phytosterols, in effect, grab and take the cholesterol in our body along with them to be passed through our digestive system and out the back end.
If we get phytosterols into our gut by eating them, less excess cholesterol gets reabsorbed, and it ends up getting dumped. This shows the increased fecal excretion of both dietary and endogenous cholesterol, when one eats a phytosterol-rich diet.
A picture is worth a thousand words, and this one shows the correlation between phytoserol consumption and the excretion of both the cholesterol produced by our body and cholesterol consumed from food sources, like saturated fats:
How Phytosterols Lower Cholesterol
You may find the original video and transcript here.
Because nuts are rich in phytosterols, they should be eaten in plenitude if you have high LDL.
In the next and final video, Dr. Greger presents a pooled analysis of 25 recently published trials investigating nut consumption and the levels of fatty substances (like cholesterol) in the blood.
The risk of heart disease was cut in half simply be eating nuts. (Watch the video.)
If your LDL starts out under 130 mg/dL (about twice what it ideally should be), then, eating nuts lowers LDL about three percent. If, however, your beginning LDL start out in the mid-100s, the nuts work twice as hard. And, if you’re off the charts, ready to keel over any moment, nuts drop your bad cholesterol an average of like ten percent.
That said, know that these nut studies were funded by industry groups, so there’s an obvious incentive to put things in a positive light.
Nuts and Bolts of Cholesterol Lowering
You may find the original video and transcript here.
Before you go, I recommend you read my article, How To Reduce Your Probability of Getting Heart Disease By 5o%. Among lot of other stuff, I write about how two great supplements, the ubiquinol form of CoQ10 and Selenium improves overall heart function.
Your Takeaway
If you bypassed this very long article to get here to the bottom line, know this:
- The most important cholesterol numbers are those associated with LDL cholesterol particle size, such as lipoprotein(a), which can be determined by a VAP test.
- You can reduce your LDL cholesterol by eating phytosterol-rich foods (such as green veggies, nuts and seeds), eating less saturated fats, exercising, losing weight and supplementing with Curcumin (reduces inflammation), Ubiquitol (a form of CoQ10) and Selenium.
P.S. If you think you may be eating the wrong combination of macronutrients (protein, fats, carbs), answer Dr. Mercola's questionnaire to see what "nutritional type" you are. At the end of the questionnaire, you can download a meal plan and other material. Click here.Last Updated on February 28, 2022 by Joe Garma