Your ApoB Level Predicts Heart Disease, Part 2
You want to know your apoB level, and a simple, cheap test will give it to you. It’s more predictive of heart disease than any other test. So, what are you waiting for!?
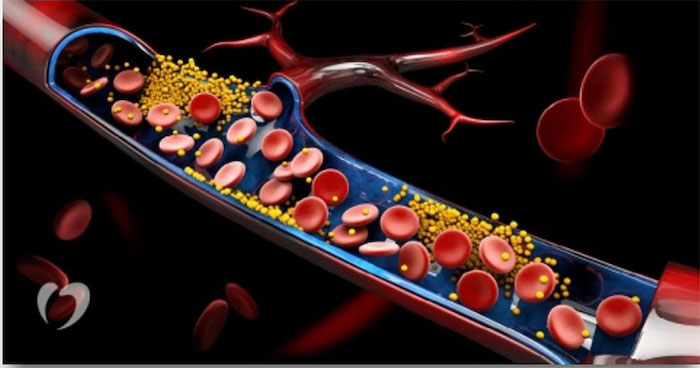
ApoB may be a more accurate risk predictor of atherosclerotic cardiovascular disease (Photo courtesy of Intermountain Health and https://www.labmedica.com/molecular-diagnostics/articles/294796425/apob-protein-testing-more-accurately-predicts-heart-disease-risk-than-testing-for-cholesterol-alone.html)
Your apoB level predicts your risk for heart disease; particularly, atherosclerosis. Heart disease kills more humans each year than anything else. Why take the risk?
When I wrote Part 1 of this two-part series, I assumed my apoB number would be just as good as those in my annual Lipid Panel. Au contraire, grasshopper — it was bad!
Here in Part 2, I will tell you about my pitiful apoB score, and what I did to reverse the tide of Atherosclerotic Armageddon.
Here’s what I cover:
- What is apoB and why it matters
- The causal relationship between apoB and atherosclerosis
- Why my apoB level was high and how I knocked it down
- What’s a high apoB number?
- What was my apoB level?
- Why so high?
- How I knocked down my apoB number
let’s dig in…
What Is apoB and Why It Matters
Apolipoprotein B (apoB) is a protein primarily responsible for transporting cholesterol and other lipids in the bloodstream. It’s a key component of low-density lipoprotein (LDL) particles, also known as “bad cholesterol.” ApoB plays a crucial role in atherosclerosis, a condition characterized by the buildup of plaque in the arteries.
High levels of ApoB are associated with an increased risk of atherosclerosis, which is the buildup of plaque in the arteries that can lead to heart disease and stroke. In fact, ApoB is considered a better predictor of cardiovascular disease risk than LDL cholesterol itself.
Lipoprotein-related atherosclerotic cardiovascular disease (ASCVD) is a complex and deadly disease. It’s the leading cause of morbidity and mortality worldwide, affecting more than 500 million individuals globally and accounting for 19 million deaths annually [1]. Knowing your risk for getting this disease is very important. ApoB is considered the ideal, if not essential, measurement to assess risk, according to recent research.
The causal relationship between apoB and atherosclerosis
ApoB has a causal relationship to atherosclerosis because LDL particles containing apoB are prone to entering the arterial walls and becoming oxidized. This triggers an inflammatory response, leading to the formation of plaques. Over time, these plaques can obstruct blood flow, potentially leading to various cardiovascular events, such as heart attacks and strokes.
Plaque buildup in arteries occurs as a result of a process called atherosclerosis. Atherosclerosis is a chronic inflammatory condition that involves the gradual accumulation of plaque within the walls of arteries. Here is a detailed explanation of the process:
- Endothelial Dysfunction: It all begins with endothelial dysfunction, which refers to impaired functioning of the inner lining (endothelium) of the arteries. Various factors, such as high blood pressure, smoking, high cholesterol, and inflammation, can damage the endothelium.
- Lipid Accumulation: When the endothelium is damaged, it becomes more permeable to lipids, particularly low-density lipoprotein (LDL) cholesterol. LDL particles, often referred to as “bad cholesterol,” penetrate the damaged endothelium and accumulate within the arterial walls.
- Inflammation and Foam Cell Formation: As LDL cholesterol accumulates, it undergoes oxidative modifications, triggering an inflammatory response in the arterial walls. White blood cells, specifically macrophages, are recruited to the site of inflammation. Macrophages engulf the oxidized LDL particles and become foam cells, creating fatty streaks within the arterial walls.
- Plaque Formation: Over time, foam cells accumulate and combine with other substances, such as smooth muscle cells, collagen, and calcium, forming a fibrous plaque. This plaque consists of a core of cholesterol and debris covered by a fibrous cap.
- Plaque Growth and Complications: The plaque can continue to grow, narrowing the arterial lumen and reducing blood flow. Additionally, the fibrous cap covering the plaque can become thin and prone to rupture. A rupture exposes the inner core of the plaque to the bloodstream, leading to the formation of a blood clot (thrombus). If the clot completely blocks the artery, it can cause a heart attack or stroke.
It’s important to note that atherosclerosis is a complex process influenced by various factors, including genetics, lifestyle choices, and other underlying health conditions. High levels of LDL cholesterol, along with other risk factors such as smoking, hypertension, diabetes, and obesity, can accelerate the development and progression of plaque formation.
There are many indicators that suggest that a person could get some form of heart disease down the road, the most common metrics being the annual Lipids Profile your doctor prescribes, consisting of cholesterol, LDL-C, HDL-C and triglycerides.
I don’t know why they bother — what you need to know is your apoB level, because this is the metric that’s causal. Take a minute to understand what this “causal relationship” to atherosclerosis means.
ApoB is considered a causal marker for atherosclerosis because it reflects the number of potentially atherogenic lipoprotein particles. This is because each particle of Very low-density lipoprotein (VLDL), Intermediate density lipoprotein (IDL), Low-density lipoprotein (LDL), and Lipoprotein(a) (Lp(a)) is carried on the surface one molecule of ApoB. ApoB levels indicate the atherogenic particle concentration independent of the particle cholesterol content, which is variable [2].
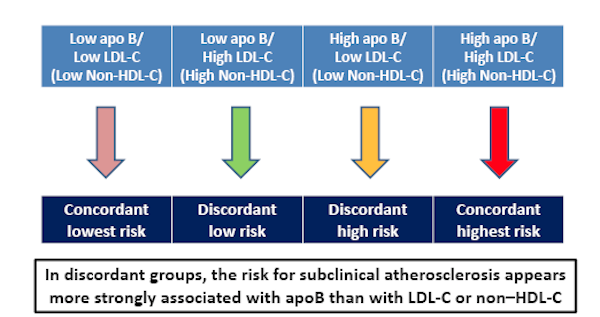
A high ApoB score, say over 100, would mean that a person has a high number of atherogenic lipoprotein particles, which can lead to the formation of atherosclerotic plaques in the arteries [3]. In most prior reports, ApoB surpassed LDL cholesterol and other cholesterol-based measures in predicting cardiovascular disease risk [4]. Consequently, ApoB is considered the ideal, if not essential, measurement to assess lipoprotein-related atherosclerotic cardiovascular disease (ASCVD) risk [3].
In an article in JAMA Cardiology, Allan Sniderman and his colleagues make the case that apoB level — rather than LDL-Cholesterol, non-HDL-Cholesterol, or even LDL particle count (LDL-P) — is the best measure of potentially atherogenic lipoproteins. LDL and HDL are also associated with atherosclerosis, but ApoB is considered a better marker of cardiovascular risk than LDL-Cholesterol [5].
If you haven’t already done so and you want to get more background information about apoB, read Part 1.
Why My apoB Level Was High and How I Knocked It Down
Typically, it takes a pretty comprehensive approach to reduce your aboB number, as you’ll soon see. But it’s so worth doing, because the higher you aboB number, the greater your risk from succumbing to the number one killer of humans worldwide.
What’s a high apoB number?
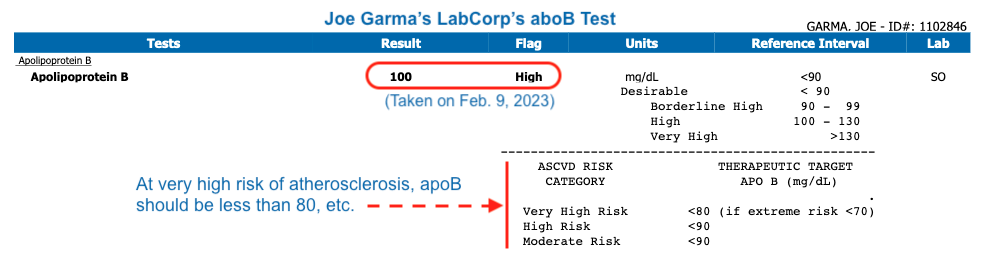
An ideal or “good” apoB score varies depending on the guidelines provided by different medical organizations; however, a commonly accepted level is below 90 mg/dL (milligrams per deciliter). This value indicates a lower risk of atherosclerotic events. On the other hand, an elevated apoB level above 100 mg/dL, and certainly at 130 mg/dL and higher, is generally considered high, indicating an increased risk of heart disease.
Mine used to be 100 mg/dL!
What was my apoB level?
I did an apoB test at LabCorp in early February of 2023 via the Life Extension Foundation. As I reported in Part 1, Why High ApoB Is A Ticket to Heart Disease:
“… how much of what type of cholesterol is streaming through your arteries matters greatly. The parsed story line that HDL is good and LDL is bad is an incomplete narrative; you need the whole story in order to act appropriately to safeguard your health.”
I also wrote that I had ordered my apoB test from Life Extension.
That Part 1 post was originally published on Oct 22, 2022. Soon thereafter, I received my test voucher, but procrastination got the better of me, and I did not go get my blood drawn at LabCorp until February 9, 2023. I got the test results back in a couple of weeks, and then after hyperventilating over the results for a few weeks, published this update in Part 1:
I finally went to the lab and got my blood drawn for the apoB test and was shocked by the score -- 100, which is crazy high. I will soon get a retest and describe my intervention program in Part 2 of this tale.
Yep, my apoB score was 100 mg/dL.
I was pretty perplexed, given that I follow the Mediterranean Diet, exercise regularly (both resistance and cardiorespiratory training), and was taking a 2.5 mg statin each day.
Why so high?
Eventually, I did find the culprit — my genetics!
ApoB levels can be influenced by genetic factors. Certain genetic variants can affect the production, metabolism, and clearance of apoB particles, leading to variations in apoB levels among individuals.
I got my DNA analysis from 23andMe years ago, and discovered:
- A 51% likelihood of developing high LDL-Cholesterol (high is not good)
- A 38% likelihood of developing low HDL-Cholesterol (low is not good)
- A 70% likelihood of developing high triglycerides (high is not good)
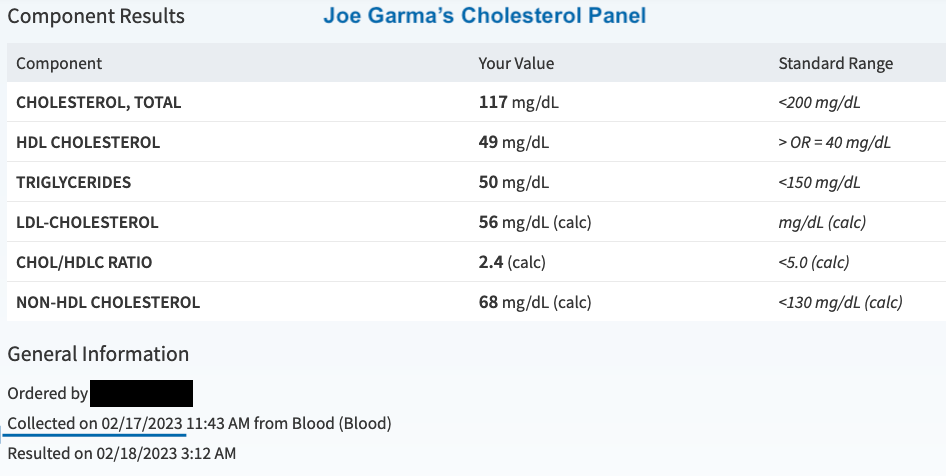
Despite that, my lifestyle factors transcended my genetics in the above three cases, as the following Lipid Panel done on February 17,2023 suggests:
Those numbers shown in the above screenshot are excellent, except for HDL, which is so-so.
But, as my high number attests, apoB doesn’t give a hoot about the regular Lipids Panel our doctors routinely prescribe, and that’s a problem. As I detailed above: You need to know your apoB number.
Even if you seemingly healthy levels of LDL cholesterol, high-density lipoprotein (HDL) cholesterol, non-HDL cholesterol, and triglycerides, you can still have a high apoB score. This discrepancy arises because apoB captures all atherogenic particles in the blood, while other cholesterol measures may not account for certain LDL subfractions that are equally atherogenic.
And that’s the case with me. As I learned a bit more than a year ago from a Quest Diagnostics’ Lipoprotein Fractionation, Ion Mobility test.
The ion mobility-derived total LDL particle concentration (nmol/L) reflects direct detection and quantitation of the total number of LDL particles. This differs from the apoB test, which measures the number of non-HDL particles, including LDL particles. I didn’t know about apoB at the time, or I just would have done that test.
Anyway, this is my LDL particle, Ion mobility test result:
Component Results
| Component | Your Value | Standard Range | Flag |
|---|---|---|---|
| LDL-P | 1,253 nmol/L | <1,138 nmol/L | H |
| LDL SIZE | 221.1 Angstrom | >222.9 Angstrom | L |
| LDL DENSITY PATTERN | A Pattern | ||
| LDL, MEDIUM | 274 nmol/L | <215 nmol/L | H |
| LARGE HDL-P | 6,182 nmol/L | >6,729 nmol/L | L |
| SMALL LDL-P | 199 nmol/L | <142 nmol/L | H |
The bottom line is that when I took that test on March 16, 2022, my LDL and HDL particle size and numbers were largely less than ideal.
And this was confirmed by the first apoB test I took at LabCorp, as shown above.
How I knocked down my apoB number
First, I did some research.
I found these various things to try to reduce my apoB number of 100 mg/dL:
Pharmaceutical Interventions
- Statins: These medications lower LDL cholesterol and apoB levels by inhibiting an enzyme involved in cholesterol synthesis.
- Ezetimibe: This medication reduces cholesterol absorption in the intestines, leading to decreased LDL cholesterol and apoB levels.
- PCSK9 inhibitors: These newer medications help lower LDL cholesterol and apoB levels by increasing the removal of LDL particles from the bloodstream.
Lifestyle Modifications
- Adopting a heart-healthy diet: Emphasize whole foods, fruits, vegetables, whole grains, lean proteins, and healthy fats, while limiting processed foods, saturated fats, and added sugars.
- Regular exercise: Engage in aerobic activities to improve lipid profiles and overall cardiovascular health.
- Weight management: Maintain a healthy weight or lose excess weight through a combination of diet and exercise.
- Smoking cessation: Quit smoking, as it contributes to endothelial dysfunction and atherosclerosis.
Supplements
- Omega-3 fatty acids: Fish oil supplements containing omega-3 fatty acids have been shown to lower LDL cholesterol and apoB levels.
- Plant sterols: These natural compounds, found in certain fruits, vegetables, and nuts, can help reduce cholesterol absorption in the gut. (See the “Note” below)
- Niacin: a B vitamin that has been shown to reduce ApoB levels in some studies
- Pantethine: a derivative of vitamin B5, which reliably lowers LDL cholesterol and the LDL carrier protein ApoB, without statin-like side effects, and without lowering protective CoQ10 levels.
- Artichoke leaf extract: raises levels of the protective ApoA carrier molecule that supports the HDL particle, which contributes to observed increases in beneficial HDL levels.
- Berberine: a plant compound that has been shown to reduce ApoB levels in several studies.
- Policosanol: a natural supplement derived from sugar cane wax that has been shown to reduce ApoB levels in some studies.
Note: Click here for a cautionary tale about Plant sterols
In the Comments below this post, “Marco” pointed out that lipidologist Dr. Thomas Dayspring recommends not taking Plant sterols. I follow Dr. Dayspring and value his opinion, so I did some research on this.
Dr. Thomas Dayspring has expressed concerns about the use of plant sterols in managing cholesterol levels.
– He has warned that dietary sterols such as phytosterols may contribute directly to atherogenesis, raising questions about their use [1].
– He has also stated that if a genetic analysis shows LOF SNPs of ABCG5/G8, one should not recommend phytosterol supplements [2].
– In an article on the Cleveland Clinic website, it’s mentioned that phytosterols are not recommended for people with sitosterolemia, a genetic disorder in which cholesterol and plant sterols build up in the body. High plant sterol levels may cause an increased risk of early atherosclerosis [3].
However, it is worth noting that plant sterols are natural compounds found in plants that can help lower cholesterol levels and reduce the risk of heart disease [3]. While phytosterols decrease LDL-cholesterol levels, there is no evidence that they reduce the risk of cardiovascular diseases [4]. Therefore, it is important to consult with a healthcare provider or dietitian to determine if phytosterol supplements are appropriate for your specific health needs.
Citations:
[1] https://twitter.com/Drlipid/status/1301512188188930050
[2] https://twitter.com/Drlipid/status/1625281461661179906
[3] https://my.clevelandclinic.org/health/articles/17368-phytosterols-sterols–stanols
[4] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5729784/
I then did some searching around about Plant sterols more broadly, not associated with Dr. Dayspring. It appears from my sources that Plant sterols are generally considered safe for most healthy people, but there are some potential risks associated with their consumption. Here are some of the risks mentioned in the search results:
– High plasma plant-sterol levels may be detrimental and associated with premature atherosclerosis [1].
– The genetic disease sitosterolemia, which is characterized by elevated plasma levels of plant sterol, is associated with premature atherosclerosis [1][2].
– Although plant sterols can block the absorption of dietary cholesterol into the body, high vegetable diets and/or plant sterol supplements can pose health risks [3].
– Some studies suggest that high plasma levels of plant sterols are associated with increased cardiovascular risk [1].
– Plant sterols can cause side effects such as diarrhea or fat in the stool [2].
– Plant sterols have no evidence of reducing the risk of coronary heart disease and much evidence that they are detrimental [4].
As mentioned, it usually makes sense to consult with a healthcare provider or dietitian to determine if Plant sterol supplements are appropriate for an your specific health needs.
Citations:
[1] https://pubmed.ncbi.nlm.nih.gov/25497968/
[2] https://www.nccih.nih.gov/health/providers/digest/high-cholesterol-and-natural-products-science
[3] https://www.sciencedaily.com/releases/2008/07/080714165856.htm
[4] https://thescipub.com/abstract/ojbsci.2014.167.169
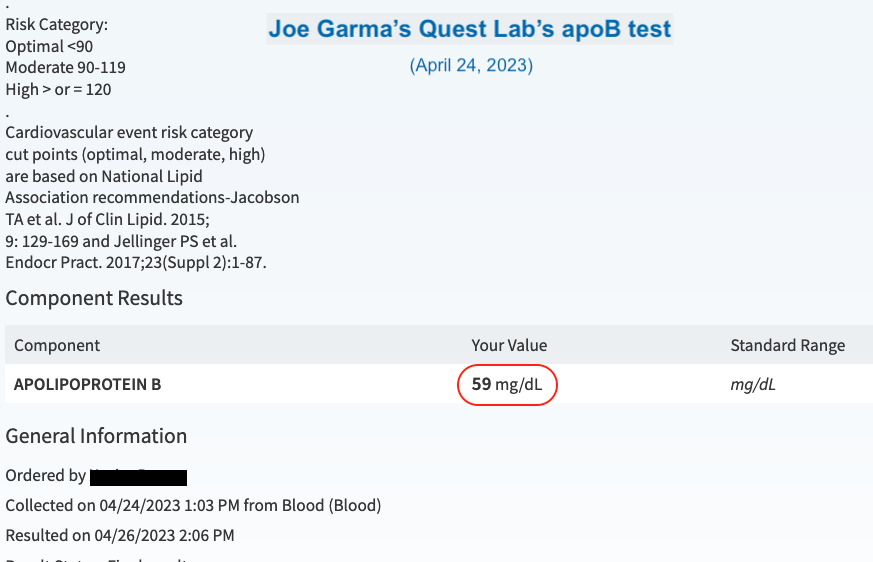
Out of that list, here’s what I did:
- Increased my statin from 2.5 to 5 mg per day
- Continued with my Med Diet and regular exercise, both cardiorespiratory and resistance training
- Kept niacin at 500 mg per day (an already high dose)
- Doubled my fish oil supplementation to 2.4 grams per day (1.2 grams twice per day)
- Doubled my plant sterols to 1 gram per day (500 mg twice)
- Reintroduced berberine to my supplement stack at 800 mg per day (400 mg twice) Note: don’t take berberine chronically; rather try one/two months on, one month off.
Two months later, I retested, this time via my doctor’s prescription using Quest Diagnostics.
I knocked my apoB level down to 59 mg/dL!
The ideal or “good” apoB score may vary depending on guidelines and population characteristics. Generally, an apoB score below 90 mg/dL is considered favorable and associated with a lower risk of atherosclerotic events. That said, many doctors who are apoB specialists say that “lower the better”.
“When you look at a lot of the Mendelian randomizations plus the clinical trial data, if you have an LDL cholesterol below 30 or an ApoB below 40 milligrams per deciliter for a very long period of time, I think the odds that you’re going to suffer for ASCVD are incredibly low.”
I plan to retest again later this year (2023). If the retested number is much lower or higher, I’ll write a post about it; otherwise, I’ll just drop a not to my Subscribers in their weekly Newsletter.
In the meantime, if your doctor won’t order it for you, get your apoB test via Life Extension. It’s cheap and very worthwhile.
That’s it… if you have questions or comments, scroll down and have at it.
Subscribe to my Newsletter!
Last Updated on July 28, 2023 by Joe Garma