How to Mimic GLP-1 for Steady Weight Loss
Mimic GLP-1 and you reduce hunger, improve glucose control and get leaner. All you need is protein and fiber. Here’s why this works and how to do it.
To mimic GLP-1 means to replicate the effects and actions of the hormone glucagon-like peptide-1 (GLP-1) in the body. The aim of this post is to show you how to do this.
Why bother?
Because GLP-1 is an important appetite-regulating hormone produced in the gut that has several key effects relevant to weight management and metabolic health, such as:
- Appetite suppression: GLP-1 helps reduce hunger and promote feelings of fullness, leading to decreased calorie intake.
- Delayed gastric emptying: GLP-1 slows the rate at which the stomach empties, prolonging the sensation of satiety after eating.
- Increased insulin secretion: GLP-1 stimulates the pancreas to release more insulin, improving glucose control.
- Decreased glucagon secretion: GLP-1 suppresses the release of the hormone glucagon, which helps manage blood sugar levels.
The goal of mimicking GLP-1 is to leverage its appetite-suppressing, glucose-regulating, and metabolic benefits to support weight loss and improve overall metabolic health in a sustainable way.
I’m going to tell you how to do this using protein consumption based upon your lean body mass and dietary fiber.
Let’s dig in…
The Problem: Your Appetite Hormone Makes You Too Hungry
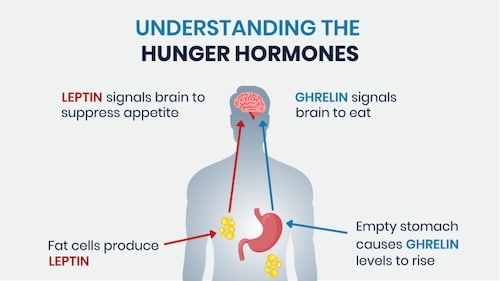
Ghrelin is the “appetite hormone” that, in effect, makes you hungry. Ghrelin is a gut-derived hormone that stimulates appetite and food intake. It’s considered the counterpart to leptin, a hormone that suppresses appetite.
We want to suppress ghrelin to a modest degree in order to control our appetite and the number of calories consumed.
The postmenopausal study
Av study published in 2016 entitled Acute and short-term effects of caloric restriction on metabolic profile and brain activation in obese, postmenopausal women investigates the early metabolic changes and brain activation patterns in response to visual food stimuli during an eight-week caloric restriction intervention. The study involved 18 healthy postmenopausal women with a body mass index (BMI) of 30–35 kg/m², which means they were obese.
Eighteen people are not many for such a study, nor is eight weeks very long, but this study’s findings are interesting. It indicated that the brain’s response to food stimuli, particularly in regions associated with reward processing, is influenced by metabolic factors and changes as a result of weight loss. This research contributes to the understanding of the relationship between diet, metabolism, and brain function, particularly in the context of obesity and menopause.
Summary of the Study:
- Objective: To examine the correlation between early anthropometric and metabolic changes with brain activity in areas involved in processing visual food-related stimuli.
- Method: Participants followed an isocaloric diet for two weeks, then a 1,000 kcal restricted diet for four weeks, followed by another two weeks on an isocaloric diet. Measurements were taken weekly during the isocaloric periods and thrice weekly during the caloric restriction.
- Results: (1) Participants experienced a mean weight loss of 4.2±0.5 kg (4.8%) and a 4.2 ±0.4 cm decline in waist circumference over the eight-week study period. (2) In the first week of caloric restriction, triglyceride, leptin, resistin and adiponectin levels as well as systolic blood pressure decreased, while insulin-like growth factor-binding protein 1 increased. (3) During and after weight loss, a significant increase in ghrelin levels was observed.
Now, you might not be an obese woman, postmenopausal or not, but the study’s findings may have some relevance to you anyway
Why?
Because the study demonstrates that favorable metabolic changes can occur rapidly with caloric restriction, even before significant weight loss is observed.
But there is a hurdle with this “caloric restriction” — hunger! Caloric restriction activates ghrelin, the hunger hormone. The study showed that the women experienced increased hunger, which could make it more difficult to maintain the weight loss long-term.
Ghrelin is a hormone that stimulates appetite, so its elevation could counteract the effects of the caloric restriction diet. This highlights the challenge of sustaining weight loss — for anyone, not just obese, postmenopausal women — and the importance of addressing the hormonal changes that occur with caloric restriction. The findings suggest the need for a strategy to manage ghrelin levels and hunger in order to support long-term weight maintenance.
The next study I’m going to tell you about suggests the strategy to overcome ghrelin. It involves a way to mimic GLP-1. Remember, that’s the road to weight management and metabolic health.
The Solution: Protein + Fiber

It seems simple, but prioritizing protein and fiber in your diet can mimic GLP-1, and thereby tamp down ghrelin and your hunger by keeping you more satiated than would other macronutrients with the same calories.
The protein/hunger study
the 2020 study entitled the Effect of short- and long-term protein consumption on appetite and appetite-regulating gastrointestinal hormones, a systematic review and meta-analysis of randomized controlled trials examines the effects of short-term (≤1 day) and long-term (>1 day) protein consumption on appetite-regulating hormones and subjective appetite in randomized controlled trials.
This study looked at two appetite-regulating hormones:
- Cholecystokinin (CCK), and
- Glucagon-like peptide-1 (GLP-1).
CCK is released from the small intestine after meals and promotes feelings of fullness and satiety. GLP-1 is also released from the gut and has been shown to reduce hunger and food intake.
The study was a meta-analysis that examined 49 publications for acute and 19 articles for the effects of protein consumption on healthy adults. It found that short-term protein consumption significantly increases levels of CCK and GLP-1 compared to control conditions.
Regarding ghrelin, the study showed that short-term protein consumption (≤1 day) had no significant effect on ghrelin levels compared to control conditions, but that for longer-term protein consumption (>1 day) it did:
“The review found significant reductions in ghrelin compared to control diets. This suggests that longer-term protein intake can modulate appetite hormones in a way that reduces hunger and promotes satiety.”
So in summary:
- Short-term protein intake (≤1 day) did not significantly affect ghrelin levels.
- Longer-term protein intake (>1 day) was found to significantly reduce ghrelin levels compared to control diets.
The reduction in this “hunger hormone” ghrelin with prolonged protein consumption helps explain why higher protein diets are often associated with reduced appetite and improved weight management. The review indicates this is likely due to the modulation of key appetite-regulating hormones like ghrelin over the longer term.
This begs the question: How much protein should you eat?
This is a complicated question to answer, because there are so many conflicting answers provided by influencers, medical doctors and academicians.
One thing is clear: The Recommended Dietary Allowance (RDA) recommended daily protein consumption of 0.85 grams per kilogram of body weight is the bare minimum. (One kilogram = 2.2 pounds.) Perhaps if you’re small, don’t move much, and don’t care about sarcopenia (age-related muscle attrition), then 0.85 is enough. The rest of us want more of it, and want to know how much daily protein to target.
The common factors to consider include your size, activity level and age, but I’m going to include an uncommon factor that hardly ever gets addressed — body fat.
Let’s look at each factor:
- Size: Naturally, the bigger you are the more protein you need, just like the other two macronutrients, dietary fats and carbs. Typically, size is accounted for by body weight.
- Activity: If you move around a lot each day, and/or consistently do aerobic exercise, you need more than 0.85 g per kg of body weight. If you consistently do resistance training (calisthenics and/or weight lifting), you need even more, because resistance training’s purpose is to break down muscle tissue in order for it to grow back larger and stronger, and you need protein for that.
- Age: We tend to need more protein as we get older because less of it gets used. This is referred to as protein muscle synthesis. When young, most of that 30 grams of protein you eat gets used, but when old you might need to consume 40 grams to use 30.
- Body Fat: As mentioned, this is rarely taken into account, but I believe it’s an important consideration. About 74% of people in the industrialized world are overweight (42% obese) [1]. I assert that the ratio of protein to body weight does not have to account for body fat.
Let’s drill down on activity and body fat in order to help you target the amount of protein to eat, not only to nourish your muscles, but to tamp down ghrelin and mimic GLP-1 and CCK, which promote feelings of fullness and satiety.
Target Protein Amount to Lean Body Mass and Activity Level
You’d be hard pressed to find a definitive source that recommends that you determine how much protein you eat relative to your lean body mass; meaning, what you weigh without the fat. But I think that’s the right way to do it for two reasons:
- Most of us would consume less protein, because most of us are overweight.
- Protein is primarily utilized by the metabolically active lean tissues, not body fat.
Using lean body mass rather than total body weight accounts for the fact that metabolically active lean tissues, not the fat mass, are the primary drivers of protein needs.
So, say you weigh 91 kg (200 lbs), your lean body mass is 68 kg (150 lbs), and you’re targeting 1.6 g/kg. You would need to consume about 146 grams of protein each day if you didn’t account for your body fat, but only 109 grams if you did. If you primarily get protein from animal products, you’d be able to eat less of it (a health benefit) and save money. Same goes for protein powder supplements. If you primarily get your protein from plants, you know that it can be hard to consume more than 100 grams per day, but taking body fat into account makes it easier.
So, what we need to target protein to lean body mass is to know how much protein is recommended irrespective of lean body mass (ie: your total body weight), and what is your lean body weight.
For sedentary adults: 0.85 – 1.2 g/kg of total body weight.
- This aligns with the Recommended Dietary Allowance (RDA) for protein, which is 0.85 g/kg for adults [2].
- You can go up to 1.2 g/kg if sedentary, but if you’re going to subtract body fat, the 0.85 number should suffice.
For older adults: 1.2 – 1.5 g/kg/day of total body weight.
From age 60 and above, aim for protein intakes of 1.2 – 1.5 g/kg/day of total body weight. If you’re doing resistance training (which you should be to avoid sarcopenia), see next.
For active/exercising adults: 1.2 – 2.2 g/kg of total body weight.
- 1.6 – 2.2 g/kg is recommended by Jäger R, et al. International society of sports nutrition position stand: protein and exercise. J Int Soc Sports Nutr. 2017;14:20 [3].
- 1.2 – 2.0 g/kg for athletes is recommended by Thomas DT, et al. Position of the Academy of Nutrition and Dietetics, Dietitians of Canada, and the American College of Sports Medicine: Nutrition and Athletic Performance. J Acad Nutr Diet. 2016;116(3):501-528 [4].
In my case, I’m an “exercising adult” who does resistance, aerobic and mobility training three to four times a week, as well as doing “exercise snacks” during the day, several days per week. My total body weight is 95 kg (209 pounds) and my body fat is 18%, which gives me a lean body mass of 78 kg (171 pounds). I’m comfortable with 1.5 g/kg of total body weight, or 142 grams of protein, because it’s reduced to 117 grams (1.5 g x 78kg) when applied to my lean body mass.
To calculate this for yourself, you need two inputs, one somewhat subjective, the other objective:
Subjective — What’s your age and/or activity level? This determines the amount of protein per weight.
Objective — Though not without error, use the Army or Navy equations below to determine your body fat, unless you can do a Dexa Scan or have an accurate body fat scale.
Use the following Army and/or Navy Fat Calculators to get your estimated body fat %, and/or body fat weight. (FYI: My results were nearly the same for each.) Then determine your lean body mass by either deducting your body fat weight from your total weight, or multipling your total body weight by (1-body fat %). Then multiply whatever grams of protein per total body weight you want against your lean body weight number.
Now that you know your daily protein target, let’s turn to dietary fiber
How much fiber should you eat?
This one is much easier to answer than the protein issue.
Dietary fiber plays a crucial role in promoting satiety and mimicking the effects of the appetite-regulating hormone glucagon-like peptide-1 (GLP-1).
I’m going to tell you why this is so by covering fiber and satiation, fiber and GLP-1 mimicry, and what are the best food and supplement sources for fiber.
Fiber and Satiation
Fiber, particularly soluble fiber, helps promote feelings of fullness and satiety by several mechanisms:
- Delayed gastric emptying: Soluble fibers like psyllium and beta-glucans slow the rate at which food leaves the stomach, prolonging the sensation of fullness.
- Increased viscosity: Soluble fibers increase the viscosity of the intestinal contents, which can delay nutrient absorption and prolong satiety signals.
- Promotion of CCK release: Fiber intake stimulates the release of cholecystokinin (CCK), a hormone that signals feelings of fullness and reduces appetite.
Fiber and GLP-1 Mimicry
Dietary fiber, especially fermentable fibers like inulin and resistant starches, can help mimic the effects of GLP-1:
- Fiber fermentation: The gut microbiome ferments certain fibers, producing short-chain fatty acids (SCFAs) that can stimulate GLP-1 release from the intestinal L-cells.
- Delayed nutrient absorption: The delayed absorption of nutrients resulting from fiber intake can also trigger GLP-1 secretion.
- Improved glucose homeostasis: Fiber’s ability to slow carbohydrate absorption and improve insulin sensitivity can contribute to enhanced GLP-1 signaling.
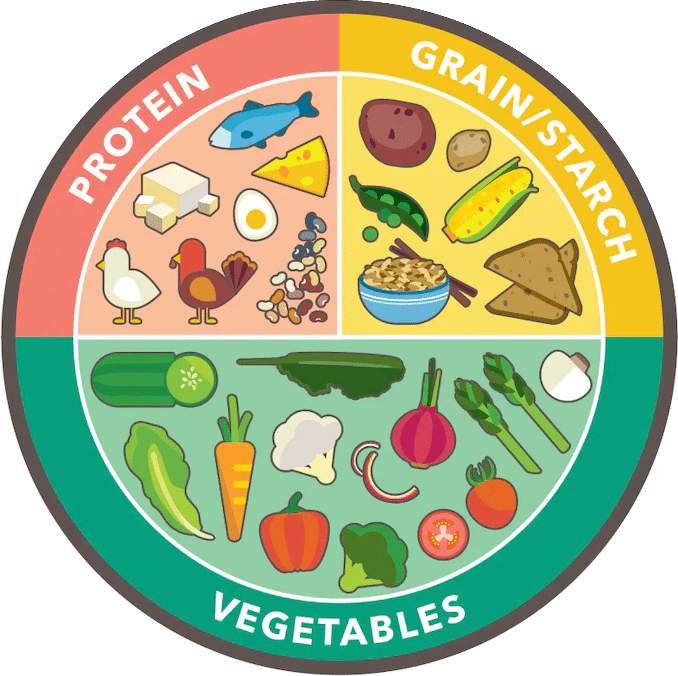
Best Fiber Sources
- Whole grains: Whole wheat, oats, barley, and brown rice are excellent sources of both soluble and insoluble fibers.
- Nuts and seeds: Almonds, walnuts, chia seeds, and flaxseeds are high in fiber and healthy fats.
- Fruits and vegetables: Berries, pears, apples, broccoli, and artichokes are fiber-rich options.
- Legumes: Beans, lentils, and peas provide a combination of fiber, protein, and complex carbohydrates.
Fiber Supplements
- Inulin: A type of soluble fiber that is fermented by gut bacteria, leading to increased GLP-1 secretion.
- Psyllium husk: A soluble fiber that can delay gastric emptying and promote feelings of fullness.
- Beta-glucans: Found in oats and barley, these soluble fibers can increase viscosity and prolong satiety.
- Resistant starch: A type of fiber that resists digestion and can also stimulate GLP-1 release.
These dietary fiber sources are crucial for enhancing the feeling of fullness and imitating the actions of the appetite-controlling hormone GLP-1. They work by slowing down stomach emptying, thickening consistency, triggering the release of CCK and GLP-1, and enhancing glucose balance. Ultimately, they contribute to maintaining healthy appetite control and managing weight.
It’s a no-brainer that you want to consciously ensure that you consume enough fiber in your diet. Aim for at least 25 to 30 grams of total fiber per day [5].
Your Takeaway to Mimic GLP-1
Mimicking the actions of the appetite-regulating hormone glucagon-like peptide-1 (GLP-1) can be a strategy for promoting steady, sustainable weight loss.
GLP-1 is a hormone produced in the gut that has several key effects relevant to weight management:
- Suppresses appetite: GLP-1 helps reduce hunger and promote feelings of fullness, leading to reduced calorie intake.
- Slows gastric emptying: GLP-1 delays the emptying of the stomach, which can prolong the sensation of fullness after eating.
- Enhances insulin secretion: GLP-1 stimulates the pancreas to release more insulin, improving glucose control.
You can mimic GLP-1 activity via adequate protein and fiber consumption, as well as regular, vigorous exercise. Chooses the level of protein grams per kilogram of total body weight you think is appropriate given your age and activity level, then to tweak it, apply that number to your lean body mass, because there’s no benefit to consuming extra protein to cover your body fat weight.
Doing all this can help you can leverage these weight-regulating mechanisms to support steady, gradual weight loss, and help prevent sarcopenia as you age.
Last Updated on April 13, 2024 by Joe Garma



