A Time Restricted Eating Study Says It Can Kill You?

Time Restricted Eating (aka Intermittent Fasting) can eventually do you harm if not kill you, reports a recent study. This upends most of the other studies about TRE. Should we be concerned?

“A Time Restricted Eating Study Says It Can Kill You?” is a provocative title, but that’s the bottom line assessment of a recent abstract of a yet-to-be published and peer-reviewed study. It concluded that long-term TRE (Time Restricted Eating) increases your chances of dying from heart problems or all-cause mortality (dying for any reason).
This has caused quite a stir!
I’ve seen multiple headlines shouting “Intermittent fasting linked to 91 percent increase in risk of death from heart disease”, or some such.
If true, we’ve been hit with a curveball, because heretofore, this time-restricted, intermittent eating stuff was thought to improve health, particularly metabolic health, which convinced a lot of people, including me, to pattern our eating this way.
Since the abstract of the Time Restricted study came out about a week ago (herein, the “study”), I’ve been asked by several people to explain what’s going on. They wanted to know if they should stop with TRE. This post is my answer,
Here’s what I cover:
- TRE/TRF vs IF
- The problem with human nutrition studies
- The TRE heart study’s findings
- A critique of the TRE heart study’s findings
- Your takeaway
Let’s dig in…
TRE/TRF vs IF
TRE is short for “Time Restricted Eating”. Many of the articles about the TRE heart study refer to it, as did the NY Times, as a study about “Intermittent Fasting”, or “IF”. This is true even though the abstract in question uses the term “Time-restricted Eating”.
The terms TRE and IF are often used interchangeably, but there are distinctions.
First off, TRE can also be referred to as “Time Restricted Feeding”, or “TRF”. In my experience in reading such studies, I find that TRF is more often the nomenclature used as opposed to TRE, but they refer to the same thing — restricting what is eaten, typically within a 24-hour period.
The real distinction, however, is not semantical. Intermittent Fasting, or IF, is applied much more broadly than TRE or TRF. For instance, IF can typically describe:
- Complete fasting for one day, or more during a week or month, or
- Complete fasting for a few days or more during a week, month or longer.
Given these definitions, it’s more accurate for the common restricted eating window of eight hours of eating and 16 hours not eating over a 24-hour period to be referred to as TRE or TRF. (I’m going to use “TRE going forward in this piece to be consistent with the jargon used by the Time Restricted study in question.) This would be true for any other combination of eating and non-eating hours during a 24-hour period.
Thus, there are different nomenclature to refer to periods of eating and non-eating, but really that’s no big deal as long as the context is clear. What is a big deal is how nutritional studies are done when the cohort being studied are humans.
The Problem with Human Nutrition Studies

Credit: Chcuk.co.uk
I’m going to expound upon some substantial problems with studies that aim to study the effects of nutrition on humans through the lens of typical TRE studies, given that they all share much of the same challenges.
Typical TRE studies on humans involve assigning participants to either a TRE intervention group or a control group. The TRE group follows a schedule where they consume all their daily calories within a specific window of time (such as eight hours) and fast for the remaining hours during the 24-hour period. The control group maintains their regular eating patterns.
The researchers then measure various health markers like weight, body composition, metabolic markers (insulin, glucose, cholesterol etc.), inflammation levels and more at multiple time points during and after the study period.
Many of these studies are of relatively short duration, from weeks to a few months. This is because enforcing strict dietary protocols for longer periods becomes challenging due to compliance issues.
While the results have been somewhat mixed, many TRE studies do show benefits like weight loss, improved metabolic health markers, and reduced inflammation compared to control groups.
However, a key limitation is that most of these are small sample sizes and not long-term studies. Nutritional research on humans in general tends to rely heavily on observational studies which are prone to confounding factors.
Human nutritional studies are observational
Nutritional research on humans tends to rely heavily on observational udies for a few key reasons:
1. Ethical and practical limitations of interventional studies:
It is often unethical to randomize people to potentially harmful dietary interventions or exposures over long periods of time. Things like assigning people to smoke cigarettes or consume excessive amounts of unhealthy foods would be unethical. Dietary intake is also a complex behavior deeply rooted in cultural and personal contexts, making it difficult to strictly control in interventional settings.
2. Studying long-term effects:
To understand the impacts of diet on chronic disease outcomes like cardiovascular disease, cancer, etc., studies need to follow participants over many years or decades. It becomes extremely challenging to maintain high adherence to specific dietary interventions over such long time frames.
3. Cost and feasibility:
Randomized controlled trials, especially large ones with long follow-ups, are extremely resource-intensive and require substantial funding and operational complexity. Observational studies can leverage existing data from large cohorts at a fraction of the cost.
Observational studies are prone to confounding factors
Observational studies, nutritional or not, are prone to various confounding factors because they cannot control the exposure of interest as tightly as an interventional study, especially with humans who, invariably, resist being put in a cage and have every aspect of their lives controlled.
Some key confounders include:
1. Healthy user bias:
People who choose to follow specific diets may also have other healthy lifestyle behaviors like exercising regularly, not smoking etc. It becomes difficult to isolate the effect of diet alone.
2. Reverse causation:
In some cases, the causal direction is unclear – i.e. did the diet cause the disease or did the disease influence dietary choices?
3. Measurement errors:
Dietary intake data collected from food frequency questionnaires or dietary recalls are prone to reporting biases and inaccuracies.
4. Unmeasured/residual confounding:
Even after adjusting for known confounders, there may be unmeasured factors like genetics, environment, etc. that affect both diet and disease risk.
Observational studies are valuable in generating hypotheses, identifying associations, and studying effects over long periods, but the potential for residual confounding is a key limitation. This is why findings from observational nutritional studies alone are typically considered as suggestive evidence until validated through well-designed interventional trials that can better control for confounding factors.
The current consensus is that TRE shows promise for weight management and metabolic health, but the overall evidence is still quite preliminary. More rigorous and long-term interventional trials are required before making definitive claims about the broad usefulness of TRE for human health.
In summary, while existing TRE research hints at potential benefits, the science is still in its early stages. Larger, longer, and more robust trials are warranted to gain greater clarity on the optimal TRE protocols and their real-world impacts on human health outcomes.
The Time Restricted Study’s Findings

Credit: Medicaldialogues.in
I’ll give you some bullet points that summarizes the study’s design, findings (including something called “Hazard Ratios”), and then tell you why the study’s conclusions were surprising,
Study Design
- Observational study using data from the National Health and Nutrition Examination Survey (NHANES) 2003-2018
- Participants aged ≥20 years who completed two 24-hour dietary recalls
- Eating duration calculated as time between first and last eating occasion each day
- Participants categorized into 5 groups based on average eating duration: <8 hrs, 8-<10 hrs, 10-<12 hrs, 12-16 hrs (reference group), >16 hours
- Mortality data obtained by linkage to National Death Index until Dec 2019
- Multivariable Cox models used to assess association between eating duration and all-cause/cause-specific mortality
Key Findings:
- 20,078 adults included, median 8 year follow-up, 2,797 all-cause deaths
- Eating duration <8 hrs associated with increased cardiovascular mortality risk (HR 1.96) in overall population
- Similar increased cardiovascular mortality risk for <8 hr eating duration in those with CVD (HR 2.06) and cancer (HR 2.72)
- No clear associations for other eating durations and all-cause/cancer mortality
- Eating duration >16 hrs associated with lower cancer mortality risk in those with cancer (HR 0.46)
Note: HR means “Hazard Ratio”, which I address below.
As noted earlier, given that the possible harm that the study indicated might befall those on TRE contradicts the basic tenet that TRE itself — irrespective of the health of the individual or healthiness of the foods consumed — is not harmful, many articles sounding the alarm have been written since the study was published (March 18, 2024). Two of them I will highlight are from the American Heart Association [1], and the New York Times [2 paywall].
Hazard Ratios
Before I summarize these articles, I want to point out something that they, and several other such articles, prominently displayed, and that is, as the American Heart Association put it in their title: 8-hour time-restricted eating linked to a 91% higher risk of cardiovascular death. The NY Times piece put it like this: Intermittent fasting linked to 91 percent increase in risk of death from heart disease.
I could not find that 91% figure in the study.
What I found was the aforementioned “Hazard Ratio”, a few of them, in fact.
The relevant line from the study states:
“Compared with eating duration of 12-16 hours, eating duration <8 hours was significantly associated with an increased risk of cardiovascular mortality (HR, 1.96 [95% CI, 1.23-3.13]);”
This means that compared to the reference group eating across 12-16 hours per day, those with an eating duration of less than eight hours had a hazard ratio of 1.96 for cardiovascular mortality risk.
A hazard ratio of 1.96 translates to about a 96% higher relative risk, not 91% higher risk.
So the abstract reports a 96% higher cardiovascular mortality risk associated with eating durations less than eight hours per day, compared to the 12-16 hour reference group. It does not explicitly state a 91% higher risk figure. Unless I’m missing something, the 91% statistic seems to be an inaccurate reporting of the results from this particular Time Restricted study. The abstract cites a hazard ratio of 1.96, which equates to around a 96% higher risk, not 91%.
Of course, nobody wants their TRE regime to increase their cardiovascular mortality risk to 91%, let alone 96% — so what’s happening here?
The surprising findings
This study, or abstract (remember that all we have to evaluate is the abstract of the study which has yet to be published) presented preliminary findings that call into question the proposed health benefits of TRE, which this review of TRE studies quoted the Salk Institute’s Satchidananda Panda, Ph.D:
“TRF [TRE] is known to improve gut microbiome, liver health, glucose regulation, muscle function (increased endurance capacity), sleep quality, cognitive function, and resilience against infectious diseases.”
This is in stark contrast with what Drs. Zong and Gardner had to say about the study’s findings, as reported in the American Heart Association article.
From lead researcher Victor Wenze Zhong, PhD:
“We were surprised that the 8-hour TRE schedule was linked to over 90% higher cardiovascular mortality risk compared to the more typical 12-16 hour eating duration. Our findings clearly show a shorter eating window was not associated with longer lifespan.
“Patients, especially those with heart conditions or cancer, should be cautious about extremely time-restricted eating based on this study’s concerning results,” Zhong stated. “While the analysis cannot prove causation, it suggests a more personalized approach is needed when recommending TRE.”
From Christopher Gardner, PhD, of Stanford University:
“This provocative data suggests time-restricted eating may have short-term benefits but possible adverse long-term effects. We need more details on factors like dietary quality to fully interpret the results, but it’s a warning about one-size-fits-all recommendations for compressed eating windows.”
As popularity of intermittent fasting diets continues growing, the researchers emphasize the need for rigorous study of long-term impacts and potential mechanisms underlying the observed elevated cardiovascular risks with a short daily eating duration.
A Critique of the TRE Heart Study’s Findings
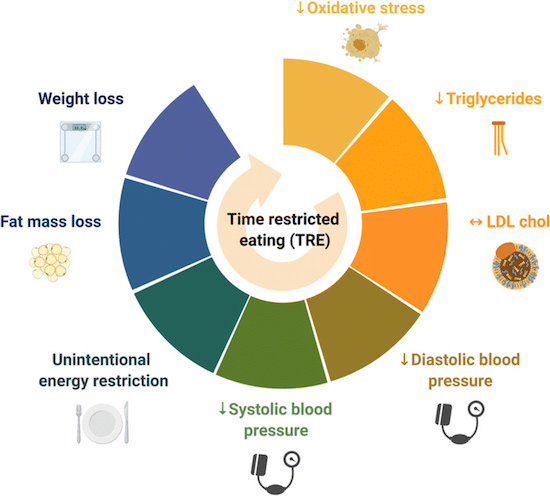
Credit: Researchgate.net / As indicated by this illustration, most TRE studies show a strong, positive correlation between TRE and various health metrics.
As mentioned, in the context of other human studies on TRE, this analysis provides some evidence that contradicts many previous short-term interventional trials that link cardiometabolic benefits with TRE regimens like 16:8 (16 hours no-eating; 8 hours eating).
That an eating window of eight or less hours per day may actually increase cardiovascular mortality risk is surprising.
But is it correct?
Human observational studies like this have inherent limitations – they cannot prove causation and may be impacted by residual confounding factors.
To establish the long-term efficacy and safety of TRE for human health, we need larger randomized controlled trials with longer follow-up periods across diverse population groups. More mechanistic studies are also needed to better understand how TRE may modulate metabolic pathways.
The New York Times article I referenced earlier interviewed Drs Vardy, Mozaffarian and Panda, all of whom suggested that — once again with human nutritional studies — there may be confounders.
Krista Varady, a professor of nutrition at the University of Illinois Chicago, said that “major limitation” is that they used just two reports to accurately represent people’s typical eating pattern; and the study did not seem to evaluate what kinds of foods people ate. And since the study has not been published or peer-reviewed, it’s challenging to fully evaluate it, Dr. Varady said.
Dr. Dariush Mozaffarian, a cardiologist and professor of medicine at Tufts University, called the study “very problematic.” The eight-hour eating group may have included many people who were very busy, or faced other challenges that forced them to miss meals or eat erratically, he said.
Our aforementioned Dr, Panda said the group could have included people who were already in poor health — those with eating disorders or illness that reduced their appetite, for instance, which may have resulted in them eating during a shorter window.
Your Takeaway
The abstract of the study that has yet to be published and evaluated found that an eight-hour TRF schedule was linked to over 90% higher cardiovascular mortality risk compared to the more typical 12-16 hour eating duration.
This is in stark contrast with most other TRF studies that show that a healthy TRF regime can improve gut microbiome, liver health, glucose regulation, muscle function (increased endurance capacity), sleep quality, cognitive function, and resilience against infectious diseases.
The problem with all such human nutritional studies is that they’re mainly observational, thus relying on participants’ reported behaviors either by interviews, or surveys.
Experts note that this particular study has limitations, including self-reported dietary data and lack of information on nutrient quality of diets across the different eating window groups. But the findings raise important questions about promoted benefits of very restrictive TRE regimens like 16:8.
Which brings me to the question: What should you do if you’re on a TRE regime?
That’s the question I’m asking myself, because I am doing the 16:8 thing. Will I change my dietary pattern? No, not yet, for three reasons:
- I want to read the full study when it comes out and judge how closely my regime and personal characteristics mirror the study’s cohort.
- If TRE is really harmful, it’s not clear why that might be. Dr. Zhong, the lead researcher, said that his study was not designed to answer that question.
- By all measures I’m healthy. None of my bi-annual blood tests, doctor check-ups and fitness level suggests that the approximately seven years I’ve been on TRF has compromised my health.
If you’re doing TRE, keep your eyes open for more research on this topic, and as always, keep monitoring your various health metrics with your doctor. Remember — what you don’t measure, you can’t manage.
For more about TRE and IF, consider reading these posts I’ve written:
- Time Restricted Feeding Improves Metabolic Health and More
- Sync Your Circadian Rhythms and Time Restricted Feeding to Optimize Health
Last Updated on April 27, 2024 by Joe Garma


