Phenotypic Aging: What It Is and How to Fight Back
Phenotypic aging is how we age. It’s how all the characteristics of aging show up. I review a study that breaks it down into four phenotypic domains with a set of associated functional outcomes — all of which decline as we get older, unless you do something about it.
Phenotypic aging is a strange expression, yet it hits the aging nail on the head. Our phenotype refers to our set of observable physical, physiological, and behavioral characteristics, which are influenced by both its genetic makeup (genotype) and its interactions with the environment.
In other words, your phenotype is the way you look, behave, and function based on your genetic traits and how they are expressed under the influence of external factors.
For example, your height, hair color, eye color, and certain personality traits are all part of your phenotype. It’s the manifestation of your genes in action, shaped by the interplay between genetics and environmental factors like nutrition, lifestyle, and exposure to various stimuli.
Keep in mind that while genetics play a significant role in determining your phenotype, environmental factors can also have a substantial impact on how your traits are expressed.
That’s a good thing, because as it turns out, how well we age is largely in our own hands.
And that brings me to what this post is all about, which is a review of a study published last year (2022) called the Longitudinal phenotypic aging metrics in the Baltimore Longitudinal Study of Aging, authored by a group of esteemed scientists, including Dr. Morgan Levine who developed the PhenoAge bioage test based on just nine blood metrics plus your chronological age.
Read on to learn the four types of phenotypic aging, how they impact us, and what to do about it.
Phenotypic aging background
The 2022 study about phenotypic aging metrics uses data from the Baltimore Longitudinal Study of Aging (BLSA), a long-term study that has been ongoing for over 60 years. The study began in 1958 and is still ongoing, making it one of the longest-running studies of aging in the world. The BLSA has followed thousands of participants over the course of their lives to study the aging process and its effects on health and functional outcomes.
The study has collected a comprehensive list of phenotypes within four domains (body composition, energetics, homeostatic mechanisms, and neurodegeneration/neuroplasticity) and functional outcomes to develop longitudinal phenotypic aging metrics. It has provided valuable insights into the complex process of aging, and emphasized the need for a comprehensive approach to improving healthspan that addresses multiple domains of phenotypes.
The study aimed to define metrics of phenotypic aging and identify biological and environmental factors that influence the pace of aging. To define metrics of phenotypic aging, it’s essential to identify biological and environmental factors that influence the pace of aging.
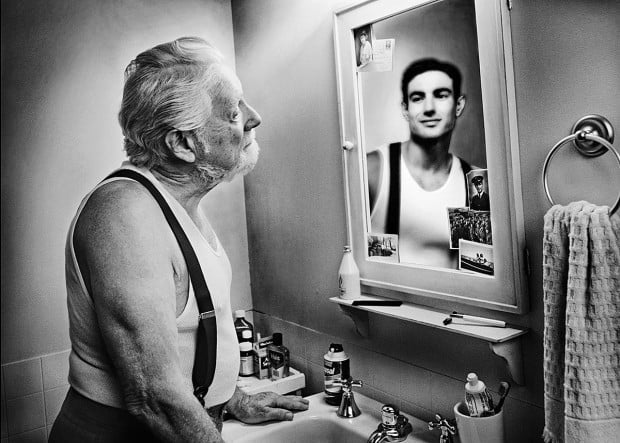
“Phenotypic aging” is like a road map of changes that happen in our bodies as we get older. It includes things like how our appearance, physical abilities, and health traits change over time. So, it’s basically a way to understand and measure how we age based on how we look, how we move, and how our health changes. Specific to the study, phenotypic aging is defined as the process of changes in phenotypes over time that are associated with aging and age-related diseases.
The “pace of aging” refers to how quickly or slowly a person’s body and health change as they get older. It’s like the speed at which different aspects of aging happen, such as changes in physical abilities, appearance, and overall health. Some people might age at a faster pace, experiencing more noticeable changes earlier in life, while others might age more slowly, with changes happening more gradually over time. We observe this every day, and such observations are part of our lexicon; to wit: You look good for your age.
To figure out how fast each person was aging, the scientists looked at how their traits changed compared to the average changes in the whole group. This helped them make a special score that shows how quickly or slowly someone is aging.
Using this aging score, the scientists discovered something interesting: People who aged faster on this score tended to have more physical and mental problems. They also got sick with multiple things more quickly and didn’t live as long. These findings were stronger compared to just looking at a person’s phenotypic traits at a single moment in time.
Let’s examine what the study reveals, and how you could benefit by them.
The four phenotype domains collected in the study, and their functional outcomes
Over many years and across a wide range of ages, The Baltimore Study collected a comprehensive list of phenotypes within four domains utilized to measure aging phenotypes; namely:
- Body composition
- Energetics
- Homeostatic mechanisms
- Neurodegeneration/neuroplasticity
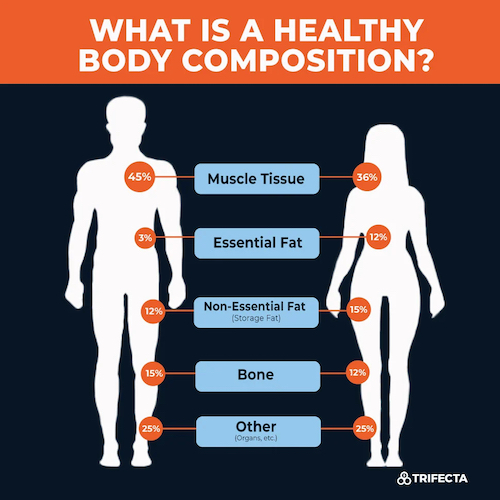
Body composition
This domain includes measurements related to body size, shape, and composition. Examples of phenotypes within this domain include body mass index (BMI), waist circumference, and body fat percentage.
The functional outcomes associated with this domain include physical performance, disability, and mortality. For example, higher BMI and body fat percentage have been linked to decreased physical performance and increased disability and mortality risk
Energenetics
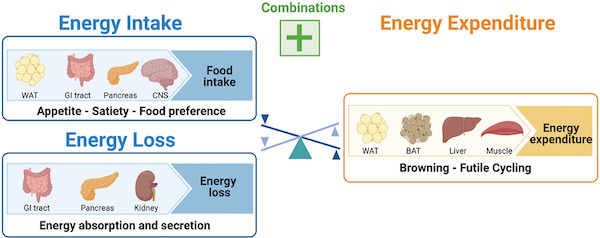
CNS = central nervous system WAT = white adipose tissue (white fat) BAT = brown adipose tissue (brown fat)
This domain includes measurements related to energy metabolism and expenditure. Examples of phenotypes within this domain include resting metabolic rate, energy expenditure during physical activity, and energy intake.
The functional outcomes associated with this domain include physical performance, cognitive function, and mortality. For example, lower resting metabolic rate and energy expenditure during physical activity have been linked to decreased physical performance and cognitive function.
Homeostatic mechanisms
This domain includes measurements related to the regulation and maintenance of bodily functions. Examples of phenotypes within this domain include blood pressure, heart rate variability, and glucose regulation.
The functional outcomes associated with this domain include cardiovascular disease, cognitive decline, and mortality. For example, higher blood pressure and heart rate variability have been linked to increased risk of cardiovascular disease and cognitive decline
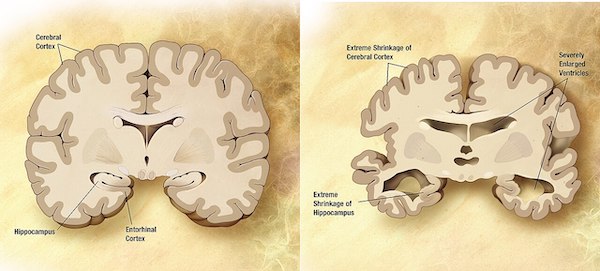
Neurodegeneration/neuroplasticity
This domain includes measurements related to brain structure and function. Examples of phenotypes within this domain include cognitive function, brain volume, and white matter integrity.
The functional outcomes associated with this domain include cognitive function, disability, and mortality. For example, lower cognitive function and brain volume have been linked to increased disability and mortality risk.
The study aimed to examine the associations between these four phenotypic domains to functional outcomes derived from the domains. It was demonstrated that the domain-specific scores using longitudinal phenotypes were robustly and significantly associated with various measures of physical and cognitive function. And that suggests that the phenotypic aging metrics within each domain can provide valuable insights into functional outcomes associated with aging.
How the functional outcomes in the study were assessed
The study assessed functional outcomes associated with aging across multiple domains. Here are some examples of how they were assessed in the study:
- Physical Performance was assessed using measures such as gait speed, grip strength, and chair stands. These measures were used to evaluate physical function outcomes, such as physical performance, disability, and mortality.
- Cognitive Function was assessed using measures such as cognitive test performance, cognitive decline, and brain volume. These measures were used to evaluate cognitive function outcomes, such as cognitive decline and cognitive test performance.
- Multimorbidity was assessed using measures such as the number of chronic diseases and the number of medications used. These measures were used to evaluate the accumulation of chronic diseases and their impact on healthspan.
- Survival was assessed using measures such as mortality rates and life expectancy. These measures were used to evaluate the impact of phenotypic aging on survival outcomes.
Overall, the study used a comprehensive approach to assess functional outcomes associated with aging across multiple domains. The longitudinal phenotypic aging metrics proposed in the study can be used to examine associations with physical and cognitive decline, multimorbidity, and survival, providing a comprehensive measure of phenotypic aging.
Were there any significant differences in functional outcomes between the four domains of phenotypes?
Yes, the study found significant differences in functional outcomes between the four domains of phenotypes. Recall that the study proposed four domains for measurement of aging phenotypes: body composition, energetics, homeostatic mechanisms, and neurodegeneration/neuroplasticity.
Here’s a summary of the relative strength of the phenotype domains associated with the functional outcomes measured :
Physical Function
The study found that body composition and energetics were more strongly associated with physical function outcomes, such as physical performance, disability, and mortality, than homeostatic mechanisms and neurodegeneration/neuroplasticity.
Cognitive Function
All four domains were weakly associated with cognitive function outcomes, such as cognitive decline and cognitive test performance. However, the associations between domain-specific longitudinal phenotypic scores and cognitive functions were weaker than that between global longitudinal phenotypic score and cognitive test performance.
Multimorbidity
The study found that accelerated longitudinal phenotypic aging across all four domains was associated with faster accumulation of multimorbidity.
Survival
The study found that accelerated longitudinal phenotypic aging across all four domains was associated with shorter survival.
Overall, the study suggests that body composition and energetics may be more important for physical function outcomes, while all four domains may be important for multimorbidity and survival outcomes.
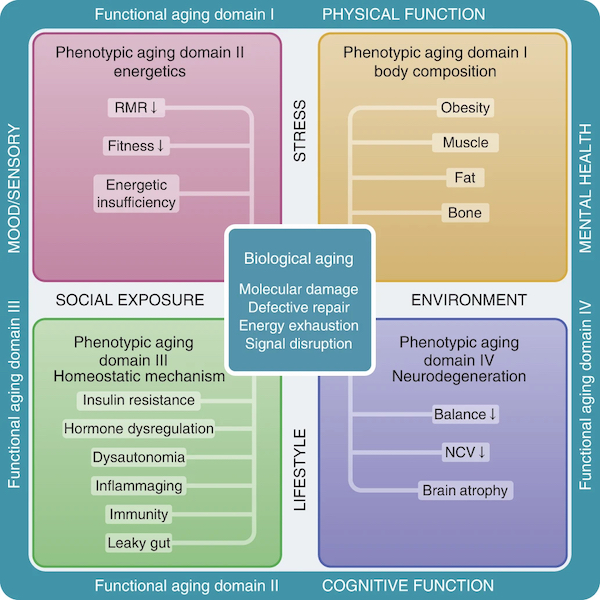
The conceptual framework underpinning the study design
To better understand the important findings of the study, let’s review its Figure 1, which illustrates the conceptual framework underpinning the study design.
The figure illustrates the hierarchical and temporal relationships between functional aging, phenotypic aging, and biological aging, based on the four domains we’ve covered earlier: body composition, energetics, homeostatic mechanisms, and neurodegeneration/neuroplasticity:
The illustration shows the conceptual framework of three hierarchical and temporal metrics of aging: biological, phenotypic and functional.
The biological mechanisms (center square) drive changes in aging phenotypes, which eventually lead to deterioration at functional levels (outer rim).
Four phenotypic domains are proposed for measurement of aging phenotypes: body composition, energetics, homeostatic mechanisms and neuroplasticity/neurodegeneration.
Examples of aging phenotypes are listed in the colored boxes. RMR is resting metabolic rate; NCV is nerve conduction velocity.
As the illustration shows:
(1) As the phenotypic aging element “energenetics” declines:
- RMR declines
- Fitness declines
- Energy declines
(2) Although it doesn’t indicate it directly, the phenotypic aging element “body composition” occurs as you:
- Gain weight (obesity/fat)
- Lose muscle (sarcopenia)
- Lose bone mass (osteoporosis)
(3) When phenotypic aging element “homeostatic mechanisms” become dysregulated, the following happens:
- Insulin resistance
- When the body’s cells don’t respond as well to the hormone insulin. Insulin helps regulate sugar levels in the blood by allowing cells to take in sugar for energy. When there’s resistance, cells don’t let sugar in as effectively, leading to higher blood sugar levels, which can eventually contribute to diabetes and other health problems.
- Hormone dysregulation
- When hormones might be produced too much, too little, or at the wrong times, which can lead to health issues or imbalances in the body.
- Dysautonomia
- When the autonomic nervous system, which controls automatic functions like heart rate, digestion, and blood pressure, doesn’t work properly. This can lead to problems with regulating these functions, causing symptoms like dizziness, fatigue, and irregular heartbeats.
- Inflammaging
- An increase in chronic, system-wide inflammation as we age.
- Immunity
- The decline in the body’s defense system against various pathogens.
- Leaky gut
- The lining of the intestines becomes more permeable than normal, allowing substances that should stay in the gut to leak into the bloodstream. This can potentially lead to inflammation and various health issues as the body reacts to these leaked substances.
(4) When phenotypic aging element “neurodegeneration” happens, the following happens:
- Balance becomes unstable
- NCV slows
- Nerve conduction velocity (NCV) is how fast electrical signals travel along nerves in your body. This measurement helps doctors understand how well your nerves are working and if there are any issues with their function.
- Brain atrophy increases
The bottom line is that pretty much everything associated with the body and mind declines as we get older. What you want to do is to slow down the decline.
How can you use this study’s findings to improve your healthspan?
Clearly, aging is a complex process involving multiple domains of phenotypes, as the Baltimore Study shows. To improve healthspan, it’ss important to take a comprehensive approach that addresses all of these domains. This may involve adopting lifestyle habits that promote healthy body composition, maintaining optimal energy levels, supporting homeostatic mechanisms, and engaging in activities that promote neurodegeneration/neuroplasticity.
There are several ways that you can apply the insights garnered by the study to improve your healthspan, none of which are surprising; however, the question is: Are you doing them?
Diet and Exercise
It’s widely recognized that diet and exercise are key factors in improving healthspan. The study suggests that interventions targeting body composition and energetics, such as maintaining a healthy weight and engaging in regular physical activity, should have a positive impact on physical function outcomes.
Incorporating a balanced diet and regular exercise into daily routines can contribute to overall health and well-being.
I’ve got some resources to help you out should you need a nudge to exercise consistently and eat healthily:
Click here to see a sampling of my posts about exercise. Click here to see a sampling of my posts about nutrition.
You might want to start by walking through my six-part series, The Functionally Fit Fast Workout. Pertinent to nutrition, eat like a Blue Zoner, or a gorilla.
Disease Prevention
The study highlights the importance of preventing chronic diseases and multimorbidity for improving healthspan. There must be a heightened emphasis to prioritize disease-free longevity and to bridge the gap between lifespan and healthspan. Few people want a long life if the last decade of it is infirmed. The goal is not just to live longer, but to live longer in good health. Therefore, focusing on maintaining physical, mental, and social well-being throughout the lifespan is crucial for improving healthspan.
This can be achieved through lifestyle interventions, such as maintaining a healthy diet, engaging in regular physical activity, managing stress, and avoiding harmful behaviors like smoking and excessive alcohol consumption.
The “Four Horsemen of the Apocalypse” are so named because most of us will die from one or more of these diseases:
- Heart disease (aka atherosclerosis)
- Type 2 Diabetes
- Cancer
- Neurodegenerative diseases (aka Alzheimer’s and Dementia)
In his best-selling book, Outlive, Peter Attia, MD, wrote about these diseases in the context of aging, which I’ve reviewed in Part 1 of my three-part series review of the book.
These are the chronic diseases that you must prepare not to get now.
Environmental Enrichment
Other studies have suggested that environmental enrichment, which includes mental stimulation, social engagement, and exposure to novel experiences, can have positive effects on healthspan.
Incorporating activities that provide mental and social stimulation, such as learning new skills, engaging in social interactions, and exploring new environments, may contribute to cognitive function and overall well-being.
Your takeaway
Longitudinal phenotypic aging metrics in the Baltimore Longitudinal Study of Aging provides valuable insights into the complex and multifactorial process of aging that is useful for those of us committed to improving our healthspan.
Here are some key takeaways:
Aging is a complex process that involves multiple domains of phenotypes, including body composition, energetics, homeostatic mechanisms, and neurodegeneration/neuroplasticity. Improving healthspan requires a comprehensive approach that addresses all of these domains.
The study found that body composition and energetics were more strongly associated with physical function outcomes, such as physical performance, disability, and mortality, than homeostatic mechanisms and neurodegeneration/neuroplasticity. Therefore, interventions that target body composition and energetics, such as diet and exercise, may be particularly effective for improving physical function and overall healthspan.
The study also found that all four domains of phenotypes were weakly associated with cognitive function outcomes, such as cognitive decline and cognitive test performance. Therefore, interventions that target multiple domains of phenotypes may be necessary for improving cognitive function and overall healthspan.
In a nutshell, the study highlights the importance of a comprehensive approach to improving healthspan that addresses multiple domains of phenotypes. Interventions that target body composition and energetics, as well as cognitive function, may be particularly effective for improving healthspan.
Any comments of questions can by typed into the Comments section below.
Last Updated on August 6, 2023 by Joe Garma