14 Ways to Wipe Out Chronic Inflammation (and why you need to)
Chronic inflammation is now considered to be the cause or amplifier of most diseases. It’s never too early to check in and ensure that your body isn’t slowly being degraded by inflammation. (Watch the videos.)
I’M ALWAYS mulling about what blog topics I might research and write for the Subscribers and stop-by visitors to this site. That’s just what was happening when I was perched on my sister’s throne during a recent visit to her home.
Right there in front of the toilet sitting pretty on top of a heap of magazines nestled in a weaved basked was a Wellness Letter published by the University of California, Berkeley. The cover article: Why inflammation is a hot topic.
“Yep, inflammation is a darn good topic”, I muttered to myself. (I endeavor to be by myself when throne-sitting.)
The reason that inflammation is a good topic is that it’s now considered to be either an antagonist of many chronic illnesses or an amplifier of them.
So, inflammation was on my mind during the last few days, and as it happens with attentional control, I started bumping into articles about inflammation all over the place:
- Dr. Dave Best wrote about it an email, Whole Body Inflammation – A Bone to Pick
- Dr. Gabe Mirken wrote about it in an article called Osteoarthritis Linked To Inflammation
- Dr. Rhonda Patrick emailed me (a subscriber) a study about how the timing and frequency of eating may influence inflammation and insulin resistance associated with breast cancer
- And, of course, the one that started this inflammation focus, UC Berkeley’s Why inflammation is a hot topic.
I read these articles and want to synthesize them and the articles I’ve previously written about inflammation in order to show you why this is something you need to check out and attend to if you have inflammation in your body.
By the way, chronic inflammation typically increases as we age, and as you’ll see is part and parcel of many chronic health issues faced during the second half of our lives.
The graph below shows how ESR (“erythrocyte sedimentation rate”), a test of inflammation, increases with age:
The intent of this article is to help you not be on that upswing curve.
In this article, you’ll discover:
- How inflammation can cause and/or amplify chronic illness.
- The symptoms and signs of chronic inflammation.
- 14 ways to wipe out chronic inflammation.
- 2 anti-inflammation fighting recipes.
Let’s dig in…
How Inflammation Can Cause and/or Amplify Chronic Illness
Before we can answer why inflammation can cause and/or amplify various chronic illnesses, let’s first identify what is inflammation.
It comes in two basic varieties: acute and chronic.
We need acute inflammation to help heal injuries. When you cut or bruise some part of your body, the area around it turns red, warms and swells. This is called an “acute inflammatory response”, because in response to the injury and infection, our immune system sends a complex array of immune cells to congregate in and around the site and release chemicals to handle the infectious organisms and debris from the injury, which then allows the tissue to repair. As the healing happens, the inflammation gradually subsides. This is all good and essential to life. (1)
Chronic inflammation is when inflammation persists irrespective of a localized injury, spreads throughout the body and affects various disease states. Unlike acute inflammation, the chronic variety is not needed at all; in fact it’s very insidious, as it can affect us quietly, can be both the cause and effect of various disorders and — as the term suggests — is and remains chronic, unless specific and consistent lifestyle choices designed to alleviate it are made.
Dr. Josh Axe says that:
When we look at the diseases that plague our society — arthritis, heart disease, diabetes, high blood pressure, asthma, inflammatory bowel disease (IBD) — we see that long-term lifestyle changes are needed. What might not be as obvious is the common denominator tied to all of them and more: inflammation is at the root of most diseases.
If you read a bit about chronic inflammation, you’ll see that last bit from Dr. Axe quite a lot:
“Inflammation is at the root of most diseases.”
For instance:
- Arthritis is inflammation of the joints;
- Heart disease is inflammation of the arteries; and
- 20% of cancer cases are linked to inflammation. (2)
Researchers have found that chronic inflammation is involved, to varying extents, in everything from coronary artery disease, cancer, obesity, and type 2 diabetes to Alzheimer’s, chronic obstructive pulmonary disease (COPD), allergic conditions such as asthma, and autoimmune conditions such as rheumatoid arthritis and inflammatory bowel disease. (3)
Dr. Tanya Edwards, director of the Center for Integrative Medicine, writes that inflammation is now recognized as the “underlying basis of a significant number of diseases.” Long known to play a role in allergic diseases like asthma, arthritis and Crohn’s disease, Dr. Edwards says that Alzheimer’s disease, cancer, cardiovascular disease, diabetes, high blood pressure, high cholesterol levels and Parkinson’s disease may all be related to chronic inflammation in the body. (4)
But how exactly is inflammation involved?
Does it cause chronic diseases, result from them, or simply accompany them (perhaps because the factors that contribute to the diseases also increase inflammation)?
Turns out, inflammation appears to play all these roles. It can be both a cause and an effect of some disorders—setting up a vicious cycle that helps explain their chronic nature.
For example, chronic inflammation plays reciprocal roles with obesity and insulin resistance. It contributes to the development of insulin resistance, which in turn may help promote obesity. Conversely, obesity worsens insulin resistance and increases chronic inflammation, partly because body fat (especially the type surrounding internal organs) releases pro-inflammatory compounds. (5)
In effect, inflammation, obesity, and insulin resistance reinforce one another and can thereby cause type 2 diabetes. Moreover, several lifestyle factors that promote inflammation, such as being sedentary and having an unhealthy diet, also promote obesity and insulin resistance.
A relatively new theory about chronic inflammation involves the human microflora—the trillions of bacteria and other organisms living in the colon, on the skin, and elsewhere in the body. Changes in the microflora caused by lifestyle and environmental factors (such as diet, antibiotic use, and air pollution) may play a role in the increase in inflammatory diseases in the industrialized world. (6)
(Read my article about inflammation/microbiota connection.)
Note that the ills above described by Dr. Edwards as being influenced by inflammation become more prevalent as we age, a situation that has coined the term, “inflammaging.” Chronic systemic inflammation is now viewed as a sort of “unified field” explanation for many, if not most, age-related chronic diseases. (7)
That hypothesis was put to the test in a 2013 study of 3,000 British civil servants published by the Canadian Medical Association Journal. A strong link was discovered between higher levels of chronic inflammation (as measured by blood levels of an inflammatory marker) and a decreased likelihood of “successful aging,” defined as optimal physical and cognitive health, and the absence of chronic diseases.
Get this — according to the study, elevated levels of inflammation:
- Reduced the odds of successful aging by half over the next decade, and
- Substantially increased the odds of cardiovascular disease and death. (8)
Click here for the link between inflammation and heart disease.
The following is from the Berkeley Wellness Report, Why Inflammation Is A Hot Topic.
For many years atherosclerosis was seen as a kind of plumbing problem—that is, merely a matter of plaque building up in the walls of coronary arteries and clogging them. But blood vessels are nothing like pipes—they are active tissue involved in complex processes. In simplest terms, cells lining the vessels absorb cholesterol (and other substances) from the blood, leading to the build-up of plaque. The body perceives this plaque as an injury and sends inflammatory cells into the vessel walls, where they set off a cascade of events that can ultimately cause plaque to rupture and a clot to form over it. If the clot breaks off or otherwise obstructs blood flow to the heart or brain, this can result in a heart attack or stroke.
It now appears that inflammation plays key roles in all stages of the development of cardiovascular disease. Bacterial or viral infection may also trigger the inflammatory process in blood vessels. Meanwhile, coronary risk factors such as obesity, high blood pressure, undesirable cholesterol levels, and smoking cause or worsen arterial inflammation. Having an inflammatory disorder, such as rheumatoid arthritis, diabetes, or inflammatory bowel disease, also increases coronary risk.
Some medications that help prevent heart attacks and strokes, notably statins, do so at least in part by reducing inflammation. The story is more complicated regarding aspirin and other nonsteroidal anti-inflammatory drugs (NSAIDs). At the low doses used to protect the heart, aspirin has only a small effect on inflammation; its heart benefit comes primarily from its ability to reduce the risk of blood clots. No other NSAIDs are good for the heart. In fact, some NSAIDs, notably celecoxib (Celebrex), increase the risk of heart attacks slightly.
Click here for the link between inflammation/cancer connection.
The following is from the Berkeley Wellness Report, Why Inflammation Is A Hot Topic.
As early as the mid-19th century, scientists found links between chronic inflammation (or its markers) and cancer. It’s now estimated that more than 20 percent of cancer cases are associated with inflammation.
Inflammation is involved with cancer development on many levels. Notably, it contributes to tumor initiation by inducing oxidative stress, DNA damage, and chromosomal instability. It promotes tumor cell proliferation and resistance to apoptosis (programmed cell death after a certain number of cell divisions, a good thing when it comes to cancer cells). Simply put, increased inflammation makes it easier for normal cells to transform into malignant cells.
The evidence is strongest concerning gastrointestinal cancers, including certain kinds of colon, liver, esophageal, and stomach cancer. It’s theorized that these organs are at high risk because they are exposed directly to pro-inflammatory dietary and environmental factors. Inflammation can also alter colonic microflora in ways that increase cancer risk.
On the positive side again, evidence is accumulating that aspirin, partly because of its anti-inflammatory effect, can reduce the risk of certain types of colon cancer and possibly certain other cancers.
The Symptoms and Signs of Chronic Inflammation
Do the following three things to determine if you might have chronic inflammation:
- Ask yourself if you over-consume sugar, saturated fats, trans fats, processed carbohydrates, artificial sweeteners and alcohol? All of these an fan the flames of chronic inflammation.
- Check to see if you’re experiencing any of these symptoms and signs:
- Constant fatigue
- High blood pressure
- Ulcers or Irritable bowel syndrome
- Allergic reactions
- Unexplained weight gain
- Ulcers
- Irritable Bowel Syndrome (IBS)
- Bloating
- Acne
- Flushing
- Water retention
- Food cravings
- Binge eating
- Diarrhea or constipation
- Joint pain
- Stiffness
- Get a blood test.
You could check “yes, yes, yes” on most of the signs and symptoms of chronic inflammation and not have it. Each item presented above could be symptomatic of another underlying issue, not inflammation per se.
The value of the list is to step you toward a blood test. If you’re experiencing any of the above signs/symptoms, do yourself a favor and get tested for chronic inflammation.
Since it is so complex, chronic inflammation isn’t measured directly. Instead, various inflammatory chemical markers in the blood or tissue are measured, notably interleukin-6, tumor necrosis factor (TNF), C-reactive protein (CRP, see inset), prostaglandins, and leukotrienes.
Elevated levels of these factors are good indicators of disease activity for some conditions (such as inflammatory bowel disease). But it’s not clear whether measuring them adequately gauges inflammation and the resulting risks for some other disorders (such as cancer).
I got a simple C-reactive protein test a few years ago, which I wrote about here. My result was was 3.74 mg/L, which is above the “reference interval” of 0.0 – 3.0 mg/L. That’s not good, nor was it obvious why I would have higher than normal chronic inflammation given that I exercise, eat like a gorilla and supplement with anti-inflammatory supplements, such as fish oil and curcumin.
Since that C-reactive protein test, I’ve been adding anti-inflammatory supplements and foods to my diet, but have yet to retest.
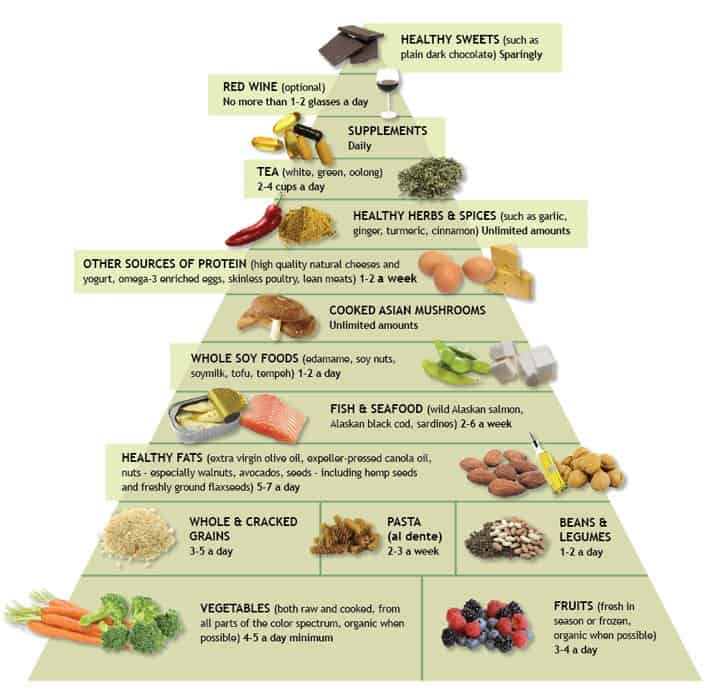
Click here to see Dr. Weil's anti-inflammatory food pyramid.
Read Why Dr. Weil’s Anti-inflammatory Food Pyramid May Be The Best Diet to get the skinny on the this anti-inflammatory food pyramid.
In addition to the C-reactive protein test, you may also elect to take the Fibrinogen test. They’re inexpensive and can be used to detect the presence of chronic inflammation and monitor the success or failure of various anti-inflammatory regimens.
| Pro-Inflammatory Marker | Optimal Ranges |
| High-sensitivity C-reactive protein (CRP) | Under 0.55 mg/L in men |
| Under 1.0 mg/L in women | |
| Fibrinogen | 200 – 300 mg/dL |
(Read about the 8 risk factors of chronic inflammation.)
The following blood tests are expensive and help identify specific factors that are causing systemic inflammation.
| Cytokine Testing | Normal Ranges (LabCorp) |
| Tumor necrosis factor alpha (TNF-α) | <8.1 pg/mL |
| Interleukin-1 beta (IL-1β) | <15.0 pg/mL |
| Interleukin-6 (IL-6) | 2-29 pg/mL |
| Interleukin-8 (IL-8) | <32.0 pg/mL |
Cytokine Panel blood test
The panel includes tests for interleukin-1 beta (IL-1ß), interleukin-6 (IL-6), interleukin-8 (IL-8) and tumor necrosis factor alpha (TNF-α), all of which are cytokines involved in inflammation that can induce damage when elevated.
This panel contains the following tests:
-
-
- Interleukin-1 beta (IL-1β) – One of the key mediators of the inflammatory response to physical stress. Higher levels are associated with anxiety, panic disorders, and cardiovascular risk.
- Interleukin-6 (IL-6) – Elevated IL-6 may occur in different conditions including chronic infections, autoimmune disorders, certain cancers and Alzheimer’s disease.
- Interleukin-8 (IL-8) – Elevated blood levels of IL-8 are associated with rheumatoid arthritis, tumor development and Hepatitis C.
- Tumor necrosis factor alpha (TNF-α) – TNF-α is a growth factor for immune cells and osteoclasts, the cells that break down bone. It may be elevated in chronic infections, certain cancers, and Hepatitis C.
-
C-Reactive Protein (CRP) Blood Test
This C-reactive protein (CRP) test indicates the degree of systemic/chronic inflammation occurring in your body. High CRP levels have been associated with cardiovascular disease, Alzheimer’s disease, diabetes and more.
Click here for more about the C-reactive protein test.
The following is from the UCB Wellness Letter, Time for CRP Testing?
![]() C-reactive protein, or CRP, is produced by the liver in response to inflammation. Of all markers for inflammation, it has gotten the most attention because research has shown that elevated blood levels are strongly associated with an increased risk of cardiovascular disease, even in people otherwise at low risk.
C-reactive protein, or CRP, is produced by the liver in response to inflammation. Of all markers for inflammation, it has gotten the most attention because research has shown that elevated blood levels are strongly associated with an increased risk of cardiovascular disease, even in people otherwise at low risk.
This was seen in the well-known JUPITER study a few years ago, which focused on people with desirable cholesterol levels but elevated CRP. It found that they greatly reduced their risk of heart attacks and strokes when they took a statin drug. Besides lowering LDL (“bad”) cholesterol, statins have anti-inflammatory effects, as seen in reductions in CRP.
Subsequently the FDA approved rosuvastatin—the statin used in JUPITER—for people who have desirable levels of LDL but high CRP and at least one other coronary risk factor. And according to revised cholesterol guidelines released last year, in cases where there’s uncertainty about statin treatment, CRP level is one of several factors that doctors should consider in making the decision.
Most doctors do not routinely measure CRP, however. It’s not clear what cutoff should be used to define high CRP, nor is it certain that bringing down elevated CRP will, by itself, be beneficial. Still, if you’re at intermediate coronary risk, and you and your doctor are on the fence about starting drug therapy, you should consider CRP testing. A high result could tip the balance toward a statin.
14 Ways to Wipe Out Chronic Inflammation
Wipe out chronic inflammation by eliminating or reducing the consumption of inflammatory foods, adding anti-inflammatory foods to your diet, supplementing with specific vitamins and herbs, reducing stress and exercising.
To help us with the particulars, I’m going to lean on Drew Canole’s article about inflammation hacks and Dr. Axe’s article about the top anti-inflammatory foods.
1. Eliminate/reduce inflammatory foods
Foods that are high in (refined) sugar and fat, wheat products and dairy are all big triggers for inflammation. Therefore, decrease or eliminate soda, refined carbohydrates and processed foods. Basically, anything that can contribute to weight gain can contribute to inflammation.
In a nutshell, EAT REAL FOOD!
Here’s a list of inflammatory foods to get off your plate:
- Sugars
- Soda
- Processed foods
- Processed meats
- Dairy
- Gluten
- Caffeine
- Trans fats
- Simple/refined carbs
- Lard
- Corn and soybean oils
- Pasteurized dairy
- Deli meat or meat from animals fed hormones and antibiotics
2. Eat omega-3 fats
Think fatty fish, seeds and nuts; these in particular:
- Salmon
- Anchovies
- Sardines
- Mackerel
- Chia seeds
- Flax seeds
- Hemp seeds
- Walnuts
All nuts and seeds contain antioxidants, which play an enormous role in the fight against inflammation by repairing the self-inflicted cell damage it causes. Nuts and seeds are a great sources of essentials vitamins, minerals, protein, fiber, amino acids and healthy fats.
3. Eat leafy greens
Cytokines are a type of small protein that play a huge role in immune response and inflammation. Vitamin E, found in spinach and Swiss chard, helps reduce the amount of cytokines in our body.
Research studies suggest that the nutrients found in dark green leafy vegetables may prevent certain types of cancers and promote heart health.
Green veggies and superfoods are rich in phytochemicals, enzymes and nutrients. Taken on an empty stomach, these nutrients can bolster and repair your cells.
Tip: Begin your day with a glass of warm water and lemon to get those digestive processes going and follow it up with a glass of green juice. See the recipes and video below.
4. Eat beets 
Another veggie super high in antioxidants, beets have been shown to fight inflammation and help thin the blood. It’s also a good source of vitamin C.
5. Eat Berries
A great source of antioxidant and anti-inflammatory properties, berries also have more fiber than most fruit and are thereby don’t spike your blood sugar as, say, gulping down eight ounces of orange juice. Try blackberries, blueberries and raspberries.
6. Eat mushrooms
Those that have potent anti-inflammatory properties include:
- Reishi mushrooms
- Maitake mushrooms
- Almond mushrooms
- Lion’s mane mushrooms
- Caterpillar fungus
- Bamboo fungus
The Host Defense brand by mycologist Paul Stamets is excellent — see these. Click here for links to studies that evaluate the anti-inflammatory effects of these mushrooms!
7. Eat garlic
Studies have shown that garlic suppresses leukocyte inflammatory cytokine production, making it a potential treatment for inflammatory bowel disease and other similar disorders.
8. Eat raw tomatoes
They contain anti-inflammatory nutrients like carotenoids and bioflavonoids.
9. Drink Tart Cherry Juice
Montmorency cherries have the highest anti-inflammatory content of any food. Research done at Oregon Health & Science University did research that says tart cherry juice may be a better and safer alternative to over-the-counter anti-inflammatory pharmaceuticals.
10. Consume these herbs:
- Turmeric — There are over 1000 different case studies showing turmeric as one of the most
powerful natural anti-inflammatory agents on the planet.
- Curcumin — It’s a compound found in tumeric and is an even more potent anti-inflammatory agent.
- Ginger — According to a PubMed, “The anti-inflammatory properties of ginger have been known and valued for centuries…” Ginger has anti-inflammatory phytonutrients known as gingerols that have been used in traditional medicine as a painkiller for arthritis and other inflammatory disorders.
- Cayenne — Contains an active ingredient called capsaicin, which is known in some cultures as a “destroyer of inflammation”.
- Ashwagandha – Sometimes referred to as the Indian ginseng, Ashwagandha root falls under the category of “adaptagen,” as it’s been shown to reduce stress and similar symptoms. Ashwagandha has also been used to treat inflammation due to the high level of withanolides. It also can help do other things, such as increase testosterone.
11. Supplement with probiotics
Aim for ten strains or more per capsule, especailly L. acidophilus or B. bifidum, which are the most potent of all the strains available.
Anywhere from 1 to 100 billion will work. Given the ridiculous amount of toxins we’re exposed to every day, many people note feeling an improvement with 20-50 billion daily. The trick is to start slow and work your way up. The typical dose for beginners is between 10-20 billion CFU’s daily.
12. Eat fermented/cultured foods
- Kimchi
- Kombucha
- Sauerkraut
- Miso
- Keifer
Fermented foods feed the probiotics you get from supplements and other foods. Kimchi, sauerkraut, kombucha and miso are going to make those 100 trillion bacteria in your GI tract very happy.
13. Exercise
The bottom line with exercise is to do what you’re willing to do.
Compliance is more important than being able to point to some praiseworthy regiment that you have to force yourself to do, and therefore do very little.
Try to move enough every day to make you winded. If you already walk, walk faster, or walk up hills.
If you jog, jog less and sprint more. 
If you lift weights, make sure you perform compound movements, like squats, and rest less between sets so you get your ticker ticking faster.
Both aerobic and anaerobic exercise have shown to decrease C-reactive protein, that marker of inflammation mentioned above. Even being active once per week was enough to lower CRP in test subjects significantly, I read somewhere, but don’t have the reference handy.
(Get inspired — Read How An Exercise Mindset and A Few Minutes Can Make You Ageless.)
14. Sleep
You deserve deep, undisturbed, restful sleep.
You spent the day working hard, eating right and exercising — now it’s time to shut off all the gadgets, sip on a cup of herbal tea, brush your teeth (don’t forget to floss), darken the bedroom completely and drift off to na na land.
Make it a priority to get adequate sleep and try to find ways to deal with stress, anxiety, and depression.
By the way, you loners should know that social isolation can also increase chronic inflammation, as was seen in a study in the Journal of Health and Social Behavior last year, so increasing social activities may help. (9)
2 Anti-inflammation Fighting Recipes
Take a look at the two videos below to see how simple it is to consume anti-inflammatory foods via juicing.
#1 Dr. Axe’s Anti-inflammatory Juice
Anti-Inflammatory Juice Recipe
Ingredients:
- 4 Celery Stalks
- ½ Cucumber
- 1 cup Pineapple
- ½ Green Apple
- 1 cup Spinach
- 1 Lemon
- 1 knob Ginger
Directions:
- Add all ingredients to vegetable juicer. Gently stir juice and consume immediately.
#2 Drew Canole’s Anti-inflammation hack-a-juice
- 2 Leaves Collard Greens
- 2 Kale leaves
- 2 Green Apples
- ¼ Hemp Seed Oil
- 1 Tbsp Apple Cider Vinegar
- 2 Knuckles of turmeric
- 1 Knuckle of Ginger
- Prepare and gather all the ingredients.
- Make sure to properly wash and clean the produce.
- Prepare the Juicer.
- Add the Collard Greens, Kale, Turmeric and Ginger into the juicer.
- Pour the extracted juice into a glass.
- Add the Hemp Seed Oil and Apple Cider Vinegar into the juice and mix well.
- Sip and enjoy your anti-inflammation juice!
Your Takeaway
Remember (and do) these five things to rid yourself of chronic inflammation:
- Each week choose one inflammatory food to expel from your diet.
- Each week add one anti-inflammatory food to your diet.
- Choose two or more anti-inflammatory supplements to regularly consume.
- Try juicing at least thrice per week.
- Move often and at a sufficient pace to get winded.
Last Updated on February 25, 2024 by Joe Garma