The Poor Performing Hormone That May Cause Your Chronic Health Problems, Part 1
Cholesterol, inflammation, high blood sugar, heart disease — What to do when you think you’re doing everything right to fix your chronic health issues, and yet they stubbornly persist? Could it be hormonal?
Note: This is article 4, part 2 to my FREE four-part series about how to build a strong and youthful body.
THERE’S A riddle I’m working on.
It’s not lyrical. It’s not particularly fun. But it is important to solve.
The riddle goes something like this:
How can a guy who religiously maintains a diet of…
- organic vegetables (steamed, soups and raw juiced),
- no-mercury fish,
- grass-fed/pastured meat (once weekly, if that),
- and complex carbs (little to no pasta, rice, sugar, bread, etc.)…
who…
- exercises every other day,
- meditates, and
- gets eight hours of sleep each night…
how can that guy have…
- Low testosterone
- High blood sugar
- Chronic inflammation
- Potential heart disease
?????????????????
That’s the riddle, and that guy is me.
This story is worth reading because it may inspire you to check your own health problems and act in a measured, consistent way to solve them.
Or at least tackle them, for these problems have not been solved. This story is an ongoing one. I believe I’m on the right track, but only time (and testing) will tell, so look for updates.
It all begins with a blood test instigated by an undesired trend.
In this tale of mystery, you’ll learn:
- Why your healthy appearance might be lying.
- Why you must get tested to know your hormone health and other health markers.
- How to peel the onion to get to the root of a health issue, cause everything is layered and connected.
Mojo-challenged
About three years ago, it dawned on me that I was living a small life. It was a comfortable life lived in a beautiful place with great friends and family, but there was no spark, or zest, or fire in the belly for doing big things.
I had wondered if I was depressed, and began reading about it. Soon, it dawned on me that my symptoms might be more descriptive of low testosterone than depression.
(At the time, I wasn’t aware that there might be something else lurking in the shadows.)
Now, if I had a big gut and flabby muscles – common symptoms of low testosterone in men past 40 years of age – I might have come to the low testosterone realization quicker. But, those weren’t my symptoms. For me it was more about attitude, about the size of the chunk of life I wanted to rip off the bone and chew.
Low testosterone in men can diminish their lives in many ways, and can be a precursor condition to many health problems, among them:
- Reduced libido and erectile dysfunction
- Diabetes
- Depression
- High blood pressure
- Fatigue and lack of energy
- Loss of muscle mass
- Increase in body fat
- Decrease in bone mass
- Mood swings (Sources: here and here.)
Like so many health issues, a big question is the questions of causality and correlation. 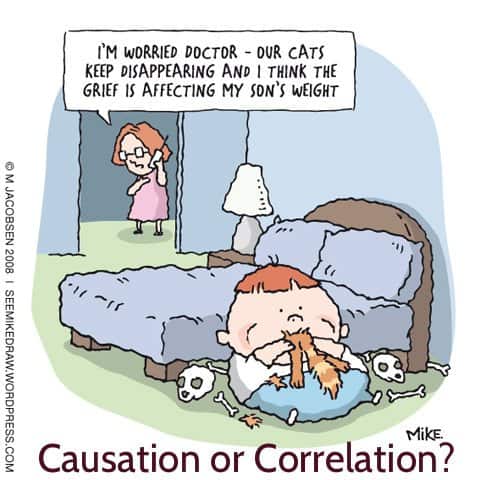
Just like it sounds, “causality” means that A causes B to happen, while “correlation” means A and B are observed together, but might have little, if anything, to do with each other.
I won’t go into a deep dive here, but these days many steadfast “truths” about health matters, such as cholesterol causing heart disease are being re-investigated and recast as being more correlated than causal.
Mini Dive
Since high cholesterol is experienced by so many, let me point out that many medical researchers are now saying that the pertinent question is about whether the cholesterol caused heart disease or is correlated with it.
Their view is that plaque in the coronary vessels is the result of chronic inflammation of the blood vessel wall. This chronic inflammation can be caused by infections, nutritional deficiencies, chemicals in food/water/environment, heavy metals (mercury, lead and aluminum), pharmaceutical drugs, hypothyroidism and low testosterone.
When there’s inflammation and damage to the arteries, the body reacts with two anti-inflammatory responses: It first tries to repair the inflammation with collagen, and – if there is insufficient amounts of vitamin C, D, L-lysine and L-proline in the body – it then resorts to using fats in the blood including lipoproteins and cholesterol. More here.
So, the question at that time for me was, is my low mojo being caused by depression or low testosterone, and which causes the other?
Know Your Blood
I decided to get a blood test called the Male Hormone Panel administered by the Life Extension Foundation (“LEF”), which I recount in posts called, Boost Your Testosterone Naturally and Look, Your Blood Reveals Your Health.
Here were the results:
| Test | My Test Result | Lab Range | LEF Range |
| Testosterone, Serum | 438 ng/dL | 348 – 1197 | 700 – 900 |
| Free Testosterone | 8.5 pg/mL | 7.2 – 24 | 20 – 25 |
| Pregnenolone | 70 ng/dL | ?* | 125 – 175** |
| Dihydrotestosterone | 27 ng/dL | 30 – 85 | 30 – 50** |
| DHEA | 67.2 ug/dL | 51.7 – 295 | 350 – 490 |
| Estradiol | 19.3 pg/mL | 7.6 – 42.6 | 20 – 30 |
*No Lab Range listed.
**This range was not found on LEF’s site, but was cited by the LEF doctor who went over the blood test results with me.
Regarding the table above, note that:
– My Testosterone, Serum, Free Testosterone and DHEA numbers are within the Lab Range, albeit on the low side, but are well below the lowest number of the range recommended by LEF, which I think are more ideal.
– My Pregnenolone and Dihydrotestosterone numbers are below the range cited by either the Lab or LEF.
– My Estradiol number is near the mid-mark of the Lab range, but just under bottom of the LEF Range. This appears to be good.
According to a study cited by LEF, men with serum estradiollevels between 21.80 and 30.11 pg/mL – the ideal range touted by LEF — had the fewest deaths. Those with estradiol levels of 37.40 pg/mL or above experienced death rates 133% above those in the ideal range, and the lowest estradiol group with estradiol levels under 12.90 pg/mL suffered a 317% increased death rate.
So, the conclusion here is that when it comes to Estradiol, a mid-range number is key.
Unhappy with most of these numbers, I had to choose among three options:
- Do nothing
- Use testosterone medication
- Use natural supplements that might increase testosterone
I chose the third option, and began with taking DHEA, Tribulus Terrestris, Magnesium Oil, Stinging Nettles and Ginseng extracts, and more protein.
(Note: I since discovered via Examine.com’s great research that Tribulus Terrestris and Magnesium Oil may not do much to boost testosterone and have stopped taking them. If you use supplements (vitamins) get familiar with their work.)
For one year I blithely continued with this protocol, increased my resistance training (weight lifting, calisthenics and high intensity interval training), and then got my blood tested again, in August 2012, about eight months ago.
This time, I also tested for various components of cholesterol, as well as markers for inflammation, blood sugar, thyroid hormone production and heart disease.
The results were mixed, with the upside eclipsed by the downside.
On the “upside”, I did improve my Steroid Hormones (DHEA and Testosterone, Estradiol):
- DHEA: from 67.2 to 315.9 ug/dl, which is now on the high side, and I’ve stopped supplementing with DHEA.
- “Free” Testosterone: from 8.5 to 10.1 pg/ml, still too low – I want it around 20, minimum.
- Total Testosterone: from 438 to 452 ng/dl, still too low – I want it around 800, minimum.
- Estradiol: this stayed about the same, from 19.3 to 22 pg/ml, pretty much ideal for a male.
(To put these numbers in context, read this good summary of Steriod Hormones and optimal levels.)
On the “downside”… well… it ain’t pretty:
- Glucose, Serum (fasting blood sugar): 100 mg/dl (potentially pre-diabetic) – I want it 85.
- Homocystine, Plasma (cardiovascular health): 11.4 umol/L (potential heart disease) – I want it below 8.
- C-Reactive Protein, Cardiac (inflammation marker): 3.74 – I want it below 0.55.
- VLDL-3, (Very-low-density lipoprotein cholesterol): 10 mg/dl – I want it below 8.
- LDL Density Pattern: “B”, abnormal – I want it “A”, normal.
- TSH (thyroid related): 3.07 mIU/L – I want it below 2.
(Note: I didn’t have all these markers tested in the first blood panel, so there’s no comparison presented.)
Needless to say, I was shocked by these results. Psychologist calls it “cognitive dissonance”. Reaching back all those years ago where in college I first heard the term, I remember cognitive dissonance is when two or more contradictory beliefs, ideas, etc. are held in one’s mind simultaneously.
I go back to my fourth paragraph above – “How can a guy who religiously maintains” all those glorious things have such shitty blood test scores? This is the dissonance tweaking my cognition.
This is the riddle.
And I have an answer, or really, more like a hypothesis. But first, let’s get our arms around what those “downside” markers cited above are about.
On The Road To Perdition
Sometimes words just pop into one’s head, like “perdition”. I like it. It’s filled with hell and brimstone and works allegorically here to underscore a fact:
If you don’t atone for sins against your body, it will die. (I’m channeling Billy Graham.)
Although in my case, I would swear on a stack of bibles that I’ve been doing the exact opposite of “sinning” against the body, given my healthy ways… and yet something’s going on to produce those worrisome blood test results.
Let’s examine what they could portend.
Diabetes
Well, dear ole Dad had it. Came to him in his sixties cause he ate crap and stayed rooted to either his sofa, or a restaurant chair.
His brother got diabetes late in life too. He ate crap, lost his lower leg due to nerve damage and poor blood circulation.
Given that neither father nor uncle were born with diabetes, theirs is called “adult-onset” diabetes, and typically happens because the pancreas is overworked in response to the insulin it attempts to produce to deal with all the sugar (and “simple” carbs) eaten that spike blood glucose (sugar) levels.
Eventually, one’s body looses its insulin sensitivity, meaning that the pancreas produces insufficient insulin to deal with the blood sugar in the blood resulting from all the high glycemic (simple) carbs ingested.
(Read What’s Making Us Fat and Sick.)
When I stare blankly at a fasting blood glucose number of 100 mg/dl — which is a high, potentially pre-diabetic level – my mind seeks the underlying cause. It makes no sense that this is based on behavior, as my diet and exercise regimes are stellar.
So, Dad and Uncle Sweeny, I ask you: Can it be genetics?
Could I have inherited an underwhelming pancreas, for instance, or something else that makes my body insulin insensitive?
Or is something else going on?
Or does a fasting blood glucose number of 100 mg/dl even matter in my case?
Unsurprisingly, there’s a story behind this, and those of you interested should read my post, Know Your Blood Sugar Numbers. Here’s the first paragraph:
“Sometimes things aren’t always what they seem. Context is important. Could it be that your fasting blood sugar number is not a problem? Well, it could depend on your post-meal and Hemoglobin A1(c) results.”
The bottom line about my fasting blood glucose number is that within the context of my good post-meal and hA1(c) numbers, I may not be heading for trouble. Nevertheless, the aim is to cut that potentially pernicious 100 fasting glucose number.
If you’re dealing with high blood sugar, I recommend you read Dr. Mark Hyman’s How To Reverse Diabetes. Yes, even if you don’t have diabetes, his recommendations apply to people with high blood sugar.
Dr. Hyman reviews what to eat, drink and suggests this big mouthful of supplements to take:
- A multivitamin and mineral.
- Calcium, magnesium and vitamin D.
- Fish oil 1000–4000 mg per day improves insulin sensitivity and cholesterol, and reduces inflammation.)
- Extra magnesium 200–600 mg per day helps with glucose metabolism and is often deficient in diabetics.
- Chromium 500–1000 mcg for proper sugar metabolism.
- Antioxidants such as vitamin C and vitamin E help reduce blood sugar and improve blood sugar balance.
- B-complex vitamins should be in a good multivitamin. Extra vitamin B6 (50–150 mg per day) and B12 (1000–3000 mcg) are especially helpful in protecting against diabetic neuropathy or nerve damage.
- Biotin 2000–4000 mcg per day enhances insulin sensitivity.
- Alpha lipoic acid is a powerful antioxidant, and at 300 mg twice per day can reduce blood sugar significantly. It also can be effective for diabetic nerve damage or neuropathy.
- Evening primrose oil (gamma linolenic acid) 500–1000 mg twice per day is important to overcome deficiencies common in diabetics.
- Use cinnamon as a supplement. One to two 500 mg tablets twice per day can help control blood sugar levels.
- Other herbs and supplements that can be helpful include green tea, ginseng, bitter melon, gymnema, bilberry, ginkgo, onions and garlic. Fenugreek can also be used to help with improving blood sugar levels, although large amounts must be taken.
- Banaba leaf (Lagerstroemia speciosa) can be an effective herb. Take 24 mg twice per day.
- Konjac fiber, such as PGX (WellBetX
) as an extra supplement, four capsules 10 minutes before meals with a glass of water. This helps reduce blood sugar after meals and improves long-term blood sugar control while reducing appetite and cholesterol.
(Get your copy of Dr. Hyman’s How To Reverse Diabetes right here.)
By the way, I consistently use everything on the list above except Fenugreek and Banaba Leaf. I intend to add konjac fiber.
Heart Disease
“Homocystine, Plasma” is a blood test marker for heart disease.
It’s a protein produced by the body, usually as a byproduct of consuming meat, and higher levels (above 10 micromoles/liter) may be associated with atherosclerosis (hardening and narrowing of the arteries) as well as an increased risk of heart attacks, strokes, blood clot formation, and possibly Alzheimer’s disease. (Source)
As noted above, I tested at 11.4 umol/L.
This number is not too worrisome if it does not increase. Homocystine levels are classified like this according to MedicineNet.com:
- 15-30 micromoles per liter as moderate
- 30-100 micromoles per liter as intermediate
- Greater than 100 micromoles per liter as severe (Source)
Nonetheless – and back to my riddle – why wouldn’t someone with my health habits have a better homocystine number, say 10 or below?
The only thing I’ve not been doing that is recommended is to reduce homocystine levels is to take folic acid and B vitamins. Now I will.
Inflammation
This is a biggie, cause inflammation is considered to be the underlying condition that enables basically all chronic disease states, including many “symptoms” of aging.
C-reactive protein is elevated in the blood when there is widespread inflammation somewhere in the body. Not the inflammation that occurs when you cut or bruise yourself, which is natural and necessary to help heal, but we’re talking about pervasive, chronic inflammation that hangs out, and gradually smothers your health.
Although the C-reactive protein is a marker for inflammation, it doesn’t indicate what is causing it. Some researchers have suggested that a chronic infection with certain bacteria or viruses may raise the C-reactive protein. (Source)
And now I return to heart disease. The C-reactive protein marker could just as easily been categorized as a marker for heart disease as inflammation.
The evidence now available indicates that inflammation and molecules such as C-reactive protein associated with inflammation may be an important determinant of atherosclerosis (“hardening of the arteries”) and heart disease. (Source)
Inflammation likely contributes to heart disease by teaming up with the LDL (“bad”) cholesterol, which is deposited in the plaques that adhere to blood vessel walls and impede blood flow.
(Although as mentioned in the “Mini Dive” above, the cholesterol may not be causal, but be present in a reaction to infections, nutritional deficiencies, chemicals, etc.)
The inflammatory process may damage these plaques, allowing tiny portions of plaque to break off into the bloodstream. These small fragments of plaque can then be swept away to lodge in small blood vessels in the heart or brain, causing a heart attack or stroke. (Source)
The bottom line here is that we should all be aware of how damaging chronic inflammation is, and work to reduce it.
Things you can do:
- Eat an anti-inflammation diet, and
- Consume anti-inflammation supplements, such as Zyflamed and Curcumin.
Frankly, I’ve been eating an anti-inflammation diet and taking the above mentioned supplements (off and on) for years, and yet still record a high C-reactive protein number.
See, this is a riddle… but let’s continue on…
Cholesterol
What an enigma is cholesterol.
Gone are the days when we can definitively say that cholesterol causes arthroscleroses and heart disease.
The history of how cholesterol came to be identified as the culprit (the causal agent) of heart disease and why some medical researchers are now considering it correlated but not causal can be explored in Chris Kesser’s eye-opening ebook, The Diet-Heart Myth.
Sufficient for this post is the assertion that not all cholesterol was created equal, some of it is actually good and necessary (“HDL”), and some parts of aren’t (“LDL”); and, in fact, some parts of the not-good kind of cholesterol are really bad.
The really bad cholesterol is VLDL-3 and LDL Pattern B.
Yeah, this is unfamiliar territory for most of us, but we need to explore it to get to the bottom of the cholesterol story.
Let’s begin with the VAP test.
One reason you may be unfamiliar with VLDL and LDL Patterns is that your cholesterol blood test you probably took did not measure them. To get what are referred to as “LDL sub-fractions”, you need a VAP test.
The VAP test will offer several cholesterol sub-fractions, but among them VLDL-3 and LDL Pattern B are the most important to know about.
From MedHelp.org we learn this:
“VLDL-3 is the densest LDL sub-fraction, and is associated with a greater risk factor for heart disease than both VLDL1 and VLDL2. When breaking down LDL, particles vary in size, ranging from small, dense “Pattern B” particles to large, buoyant “Pattern A” particles. Smaller LDL particles are associated with an increased risk for heart disease. Small, dense LDL (“Pattern B”) is associated with insulin resistance or diabetes.
“Simply put, VLDL-3 is the smallest and most dense particle of LDL (Bad cholesterol) in your system. It is more prone to collect in an artery and is less likely to bind with HDL to be removed from your blood”. (Source.)
My VLDL-3, at 10 mg/dl , is high and I test Pattern B for LDL particles, which are the small, dense particles that do the most damage within arteries.
So, what can I do?
Back to MedHelp.org:
“… statins are very effective when used along with lifestyle changes that include exercise and diet. By lowering your triglyceride levels, you also lower your VLDL cholesterol levels. Healthy lifestyle changes such as losing excess weight and exercising regularly can help lower triglyceride levels. Also, avoid sugary foods and alcohol, which have a particularly potent effect on increasing triglycerides.” (Source.)
OK, great. Back to the riddle, cause I don’t have excess weight (well, maybe losing five pounds would give my abs more expression), don’t eat sugary foods (save 80% cacao bittersweet chocolate), drink modestly about once a week and have a good triglyceride number – 82 mg/dl.
(Here’s a guide to cholesterol numbers. Learn more about VAP and Cholesterol sub-fractions here at About.com.)
The pertinent question then is:
If I’m already doing all the right things, what’s left to do to reduce my VLDL-3 and change my LDL Pattern B to Pattern A, those soft, fluffy particles that bounce off artery walls rather than cutting into them?
Typical Answer:
Tweak the supplements and diet.
There’s not much more I can do with diet, except what may be one major thing, something that I’ve changed in my diet over the last year-plus:
Reduce my consumption of saturated fat.
A bit over a year ago, I began consuming the so-called “Bulletproof Coffee” made popular by Dave Asprey, the fella behind The Bulletproof Executive website. I write about it, red meat and saturated fat in and article appropriately entitled, What You Need To Know About Coffee, Saturated Fat And Red Meat.
Suffice to say that bulletproof coffee is high quality coffee blended with grass-fed butter and organic coconut oil (or MCT oil). The pitch is that, contrary to traditional medical admonishment against saturated fat, these fat sources are actually good for you and along with the high quality coffee will fuel your energy requirements for hours each day.
I was skeptical, but aided by the aforementioned Chris Kresser’s review of the literature and his own support for grass-fed butter and organic, cold pressed coconut oil, I tried bulletproof coffee.
I liked it.
It became a bit of a habit.
But, irrespective of what Dave Asprey and Chris Kresser views are about saturated fat, might it be responsible for my dismal cholesterol sub-fractions?
If so, part of the answer to how to make these cholesterol numbers better may be to drop the butter and coconut oil, two things that for the great majority of my life were rarely consumed.
Which then leaves supplements.
What supplements could I take to help reduce VLDL-3 and make those Pattern B particles big and fluffy?
A review of the literature provides the following cholesterol-reducing supplements:
- Niacin (Vitamin B3)
, full-flush kind* √
- Indian Gooseberry
√
- Green Tea
√
- Fish Oil
√
- Garlic
√
- Ubiquinol CoQ10
√
- Red Yeast Rice
(*Be careful with the amount of the full-flush Niacin you use, as it dilates the small blood vessels beneath the skin’s surface, which can be uncomfortable.)
The checked (√) supplements are the ones I’ve used.
Yep, have tried nearly all of them, but now am only consistently using garlic, CoQ10, green tea and fish oil.
I was taking Indian Gooseberry (also called “Amalaki”), but discontinued its use once I formed what might become the answer to my riddle, which segues into the last health condition flagged by my blood test…
Thyroid
OK, I’ve hinted that I had an answer to my riddle – or more accurately, a hypothesis – and now, finally, I’m going to reveal it.
My TSH blood test results first open my eyes to the possibility.
TSH is the acronym for “Thyroid Stimulating Hormone”, a hormone that is made and released by the pituitary gland. The pituitary can sense whether there is enough thyroid hormone in the bloodstream, and it releases TSH when it detects insufficient thyroid hormone.
TSH rises when the thyroid is under active because the pituitary gland is releasing more hormone to try to get the thyroid to respond and produce more thyroid hormone.
If the pituitary senses that there’s too much thyroid hormone circulating, it slows down or even stops releasing TSH, which means the thyroid is no longer getting the message to release hormone, and thyroid hormone production will slow down.
Conceptualize it like this:
Endocrinologists have determined a new, more narrow acceptable range of TSH production:
0.3 to 3.0 mIU/L. (Source.)
TSH below 0.3 is indicative of hyperthyroidism (thyroid produces too much thyroid hormone) and above 3.0 is indicative of hypothyroidism (produces too little).
It’s estimated that more than 12% of Americans are outside the acceptable range, and may be experiencing a wide array of health problems as a result, such as these for hyperthyroidism and these for hypothyroidism.
We’re talking about 38 million people, and I may be among them.
With a TSH of 3.07 mIU/L, I may have hypothyroidism, an under active thyroid. This could explain the riddle… why a person with my excellent health habits could nevertheless have worrisome blood test, which if you recall, produced these perfidious results:
- High fasting blood sugar, potentially prediabetic
- High Homocystine, a marker for heart disease
- High C-Reactive Protein, a marker for chronic inflammation, a precursor to most chronic disease states
- High VLDL-3 and LDL Pattern B, markers for arteriosclerosis
Conclusion
Hormones are powerful and you need to know yours.
You may be doing everything right with your health habits – as I think I am – and yet if any of your hormones are over or under working, your health will falter.
You will get nowhere and quickly fatigue when swimming against a strong current.
We need our hormones to be as optimized as possible to maximize our health potential, and live a long and strong life.
That certainly is my intention, and in Part 2, I’ll reveal:
- What simple tests I did to support my hypothesis that I have hypothyroidism;
- Why I think my low functioning thyroid may be the reason for those poor blood test results; and
- The protocol I’ve established for producing more thyroid hormone.
Stay tuned. Here’s Part 2.
P.S. If you like articles like this, get on the Newsletter List.
If you liked this article and want to read the rest of the series, go here!
Last Updated on July 7, 2023 by Joe Garma



