How To Test Your Insulin Sensitivity and Why It Matters
Yes, test your insulin sensitivity, because most of us have less than optimal metabolic health, and that can be a big problem leading to body fat, chronic inflammation, the feminization of men and the masculinization of women.
How to test your insulin sensitivity is part of Fuel, one of five modules from the "age-proof" online video course I'm sharing as I develop it, sans the video. If you're not already a Subscriber, click here to be notified when the course goes live.
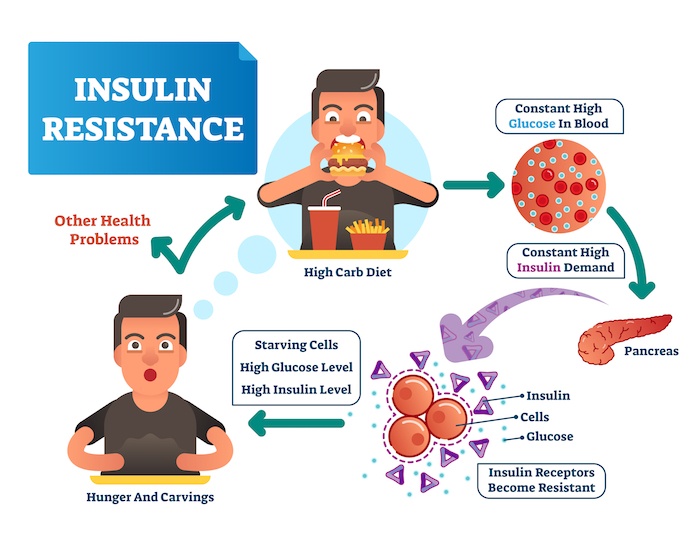
To test your insulin sensitivity is to get a big leg up on your metabolic health, because as you’ll soon learn, the odds are that your pancreas is producing too much insulin (insulin resistance), which is causing several downstream health issues, such as high blood sugar, high blood pressure, body fat, and a few more unwanted health effects that can lead to metabolic syndrome.
Take a few minutes to read how to test your insulin sensitivity, or lack thereof, and what to do about it. I also have included a VERY informative video where Dr. Mark Hyman interviews metabolic expert Dr. Ben Bikman.
Here's what's covered:
Insulin Resistance Leads to Metabolic Syndrome
According to researchers at the University of North Carolina at Chapel Hill’s Gillings School of Global Public Health, only 1 in 8 Americans is achieving optimal metabolic health, which carries serious implications for public health, not to mention the health of the great majority of Americans. (I doubt the numbers are much better in most countries in the world.)
Poor metabolic health leaves people more vulnerable to developing Type 2 diabetes, cardiovascular disease, and other serious health issues associated with impaired metabolism.
The study presents the most updated United States data on metabolic health, which is defined as having optimal levels of these five factors without the use of medication:
- Blood glucose,
- Triglycerides,
- High-density lipoprotein cholesterol (LDL),
- Blood pressure, and
- Waist circumference.
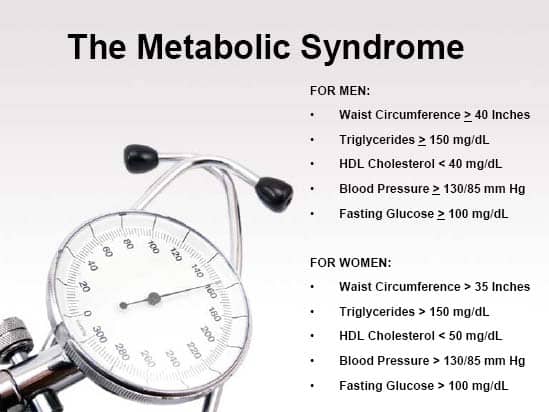
The UNC researchers examined metabolic fitness through the lens of metabolic syndrome. These are the biomarkers of metabolic syndrome:
Metabolic Syndrome is an umbrella name for a collection of health risk factors — high blood pressure, high blood sugar, high triglycerides, low HDL cholesterol, high LDL cholesterol, and excess belly fat.
If you have only two of these markers out of balance you double your risk of early death. With four markers you increase risk of death by more than threefold [1].
The primary instigator of metabolic syndrome and all of its underlying factors is INSULIN resistance!
And insulin is most impacted by glucose, which is what all those carbs we eat turn into once digested. Controlling glucose is so important to health, that longevity expert Peter Attia, MD, says,
Controlling glucose is more important than your diet.
Read "Why Controlling Glucose Is More Important Than Your Diet”, says Dr. Attia.
Now that I (hopefully) have grabbed your interest, let’s explore how insulin works, and the mess it makes if it doesn’t.
How Insulin Works (or Doesn’t) and Further Downstream Effects
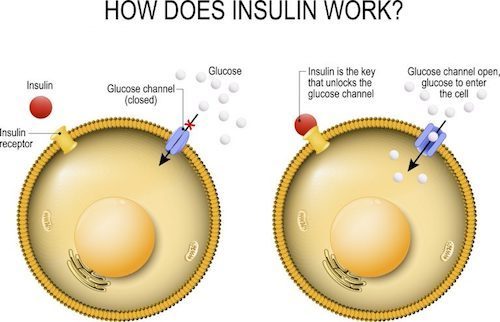
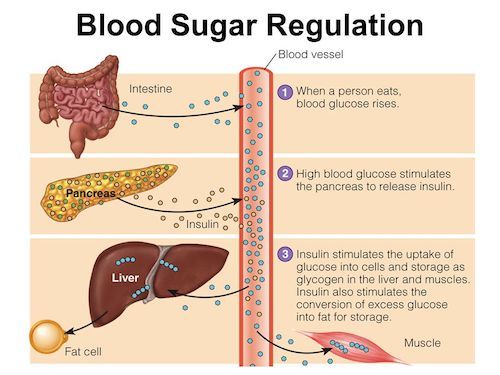
Insulin is a hormone produced by the pancreas. Insulin allows the cells in the muscles, fat and liver to absorb glucose (sugar) that’s in the blood. The glucose serves as energy to these cells, or it can be converted into fat when needed. Insulin also affects other metabolic processes, such as the breakdown of fat or protein.
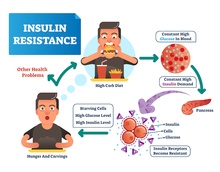
Insulin sensitivity refers to how sensitive the body’s cells are in response to insulin. High insulin sensitivity allows the cells of the body to use blood glucose more effectively, reducing blood sugar. Insulin resistance refers to the body’s cells are relatively unresponsive to normal insulin secretions, making the pancreas produce more and more insulin in order to make cells absorb glucose.
Insulin sensitivity is maintained by eating very few fast-absorbing carbohydrates (bread, pasta, fast food), and a caloric input (from food and drink) that’s equal to caloric output (from Basal Metabolism, physical activity and thermogenesis, the body’s production of heat).
The Primary Causes of Insulin Resistance
According to metabolic scientist Dr. Benjamin Bikman (see the video below), the three primary causes of insulin resistance are:
- Elevated insulin (the more it’s elevated, the more resistance)
- Elevated stress hormones, and
- Elevated inflammatory proteins or cytokines.
These are primary causes, says Dr. Bikman, because each of them can cause insulin resistance in all three biomedical models: in the cell on a petri dish, in rodents and in humans.
Dr. Bikman goes on to say in the video what he describes insulin resistance as a coin with two sides:
- One side is altered insulin signaling
- The other side is hyperinsulinemia
Altered Insulin Signaling happens when the insulin hormone is no longer acting as it used to at various cells in the body, which is the insulin resistance at the level of the cell. In this case, the insulin receptors, which every cell has, are no longer receptive to do insulin’s bidding, and lets glucose enter the cell.
Hyperinsulinemia happens when elevated insulin is chronic, and hence, doesn’t subside.
Insulin resistance creates negative downstream heath effects beyond metabolic syndrome. Two worth highlighting are health impacts to:
- The liver, and
- The sex hormones.
Insulin Resistance and the Liver
Like with all tissues in the body, insulin doesn’t tell the liver to take in the glucose, but does tell it what to do with it once it’s in liver cells, which is to store glucose and inhibit glycogen breakdown. (Glycogen is the main storage form of glucose in the body. Glycogen functions as one of two forms of energy reserves, glycogen being for short-term, and the other form being triglyceride stores in adipose tissue (i.e., body fat) for long-term storage.)
So, even if insulin and blood glucose levels are high, when the liver becomes insulin resistant, it doesn’t get the message to store glucose. Glucose keeps getting pumped out, further amplifying glucose levels, which then is further pushing up the insulin, resulting in a vicious cycle.
Insulin Resistance and Sex Hormones
Insulin resistance inhibits the ability of aromatase to do its job of converting androgens into estrogens.
Aromatase is an enzyme that converts androgens into estrogens. An androgen is any natural or synthetic steroid hormone that regulates the development and maintenance of male characteristics by binding to androgen receptors, which are on the X chromosome in a diverse range of tissues. Estrogen is a category of sex hormone responsible for the development and regulation of the female reproductive system and secondary sex characteristics.
All estrogens where once androgens. They come from testosterone, and it’s aromatase that mediates the conversion to estrogen.
Insulin resistance inhibits aromatase’s ability to convert these sex hormones. In this situation, a woman’s ovaries that are desperately trying to convert testosterone to estrogens can not, so her estrogens are too low, and she has an abnormal ovulatory cycle leading to polycystic ovary syndrome. Simultaneously, her androgens, her testosterone levels, are too high, which is what can give a woman more facial hair or coarse hair, acne, and even male pattern baldness.
Insulin resistance makes men into women, kinda. When a man’s subcutaneous fat cells are expanding, his fat cells start to express higher and higher levels of aromatase, that same enzyme that women have at high levels in her ovaries. It’s almost like his fat cells begin to act like ovaries, converting testosterone into estrogen.
In the video, Dr. Hyman jokes that:
“… with too much sugar and starch from your diet, by the time women are 65 and men are 65, they look about the same because the women get hair on their face and lose the hair on their head and men get breasts and lose the hair on their face.”
Because their estrogens are tamped down due to the impact of insulin resistance, their sex hormones tell the body where to store fat where the men store it — in the belly.
And now I think it’s a good time to show you an excellent eye-opening video of Dr. Bikman being interviewed by Mark Hyman, MD about insulin and metabolism. As I mentioned at the outset, the odds are that you’re metabolically impaired to some degree, and so I encourage you to watch the video. In the rest of the post, I’ll continue referring to remarks made in the video.
Click here for video topics and time stamps
-
The common driver of metabolic syndrome and chronic disease
-
What is insulin resistance and why is it so underdiagnosed?
-
How insulin resistance affects the liver, sex hormones, weight gain, aging, and the brain
-
Differences in how high-carb and low-carb diets affect metabolism
-
Three primary causes of insulin resistance
-
Fat, saturated fats, and insulin resistance
-
How to know if insulin resistance is a problem for you
-
Ethnic disparities in metabolic predisposition
-
Top things you can do to prevent and reverse the effects of insulin resistance
-
Insulin’s role in mTOR, a regulator of aging
How To Test Your Insulin Sensitivity
Before I get into how to determine if you’re insulin resistant, realize that it’s hard to know if you are or not by your appearance, or even by your fasting glucose and/or average glucose (HbA1c) numbers.
This is underscored by a story that Dr. Hyman tells at time stamp 06:58 in the video above. He describes a rotund, apple-shaped patient who he was sure was pre-diabetic. But he tested her glucose fasting and HbA1c numbers, and they were perfect. So, Dr. Hyman did a glucose tolerance test and, more importantly, an insulin test, which showed that her insulin levels were out of control.
Check out Life Extension's Glucose Tolerance Test with Insulin
Once his patient became insulin sensitive by doing some of the things I’ll review in the next section, she lost weight and her apple shape.
The moral of this story is that fasting glucose and average glucose (HbA1c) is important, but doesn’t tell the whole story. You also need to know insulin levels.
You can measure your insulin sensitivity through a blood test or by tape measure. The blood test is more accurate, but it costs money and takes more time. My suggestion is that you first use the tape measure, and if that indicates insulin resistance, get a blood test to confirm or deny.
Measure Your Insulin Sensitivity via Tape Measure
There are two ratios that can indicate if you’re insulin resistant:
To measure your waist-to-hip ratio:
- Stand up straight and breathe out. Use a cloth tape measure to check the distance around the smallest part of your waist, just above your belly button. This is your waist circumference.
- Then measure the distance around the largest part of your hips — the widest part of your buttocks. This is your hip circumference.
- Calculate the ratio by dividing your waist circumference by your hip circumference.
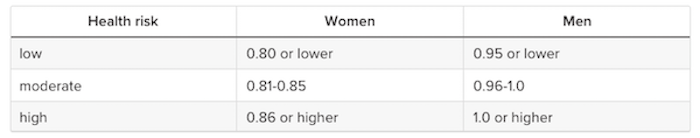
According to the World Health Organization (WHO), a moderate waist-to-hip ratio is:
- 0.9 or less in men
- 0.85 or less for women
Where are you on this table?
To measure your waist-to-height ratio:
- Use a cloth measuring tape, and measure halfway between the top of your hip bones, and the bottom of your rib cage (which for me is just over my belly button).
- Stand up straight, breathe in deeply, exhale, relax (don’t suck in your waist) and then see what the tape measure tells you.
You want your waist-to-height ratio to be half your height; ideally less.
I’m 75.5 inches tall and my waist circumference is 36.5 inches, so: 36.5/75.5 = 0.48, which is a tad under half my height (0.50).
Interestingly, WHR is a valuable indicator and predictor of your health and lifespan, which I cover in What Your Waist to Height Ratio Reveals About Your Health and How A Plant-based Diet Can Improve It.
Measure Your Insulin Sensitivity via Blood Test
The three blood tests to consider are: 
- The triglyceride-to-HDL ratio
- The NMR
- The Glucose tolerance test with Insulin
The triglyceride-to-HDL ratio
Insulin controls the production of fats and the regulation of lipoproteins in the body. A lipoprotein is a biochemical assembly whose primary function is to transport hydrophobic lipid molecules (also known as fat) in blood plasma or other extracellular fluids.
Triglycerides and HDL are lipoproteins. Triglycerides are a major component of very-low-density lipoprotein (VLDL), and HDL (high-density lipoprotein) is known as the “good” cholesterol, because it carries cholesterol from other parts of the body back to the liver that then removes the cholesterol from the body. Consequently, the triglyceride-to-HDL ratio can provide a good insight about insulin resistance.
According to Dr. Bickman, a person with a triglyceride-to-HDL ratio above 1.5 is likely to be insulin resistant. If your triglyceride HDL ratio is lower, that’s a good sign that you’re insulin sensitive.
The cholesterol panel you get with your annual blood test prescribed by your doctor will typically show HDL and triglycerides, if not the actual ratio.
NMR LipoProfile
The NMR LipoProfile® or NMR blood test is highly recommended by both Dr. Mark Hyman and Dr. Peter Attia (it’s one of his five important blood tests he recommends).
NMR look at not just the total numbers of the weight of cholesterol, which is your milligrams per deciliter, but at the particle number and the particle size, which is really important.
When you have insulin resistance, you may have get a normal cholesterol of 150, but your triglycerides may be 300 (way high), or HDL could be 30 (way low). Your doctor says, “Oh, your cholesterol is fine. Your LDL is fine.” But this might not be the case, because you may actually have really dangerous small particles that do more damage.
The Glucose tolerance test with Insulin
I’ve already mentioned this one. If you could do one blood test to test for insulin resistance, choose the Glucose Tolerance Test with Insulin, because it measures glucose and insulin prior to glucose consumption, and every hour thereafter for three hours — showing how your body responds after a meal.
OK, so at this point you know that the odds are you could improve your insulin sensitivity, you know why it’s important, and you know how to test if you’re insulin resistant. The next step is to do what’s needed to make your insulin sensitive.
How to Make Your Insulin Sensitive
A thousand calories of Coke and a thousand calories of broccoli burned in a laboratory will release the same amount of energy.
But all bets are off when you actually eat the Coke or the broccoli. These foods have to be processed by your metabolism (not a closed system). Coke and broccoli trigger very different biochemical responses in the body—different hormones, neurotransmitters and immune messengers.
The Coke will spike blood sugar and insulin and disrupt neurotransmitters, leading to increased hunger and fat storage, while the thousand calories of broccoli will balance blood sugar and make you feel full, cut your appetite and increase fat burning.
Same calories—profoundly different effects on your body.
If we make too much insulin, it drives the fuel in our blood into our fat cells. Too much insulin also does a lot of other bad things like cause heart attacks, high cholesterol, type 2 diabetes, cancer and dementia.
When it comes to causing spikes of insulin that start this miserable chain reaction, not all calories are created equally. Sugar and refined carb calories are the culprits. Americans eat, on average, about 152 pounds of sugar and 146 pounds of flour a year (almost a pound of sugar and flour per person per day!).
Here’s what you need to do to sensitize your insulin:
- Eat foods with a low glycemic load
- Practice time restricted eating
- Exercise
- Reduce stress
- Supplement
Eat Foods with a Low Glycemic load
The glycemic index (GI) is a value used to measure how much specific foods increase blood sugar levels. Foods are classified as low, medium, or high glycemic foods and ranked on a scale of 0–100. The lower the GI of a specific food, the less it may affect your blood sugar levels.
More important than knowing the glycemic index of the foods you regularly eat, however, is the gylcemic load of such foods.
According to Wikipedia, the glycemic load of food is a number that estimates how much the food will raise a person’s blood glucose level after eating it. One unit of glycemic load approximates the effect of eating one gram of glucose. Glycemic load accounts for how much carbohydrate is in the food, and how much each gram of carbohydrate in the food raises blood glucose levels. Glycemic load is based on the glycemic index (GI), and is calculated by multiplying the grams of available carbohydrate in the food by the food’s glycemic index, and then dividing by 100.
Check out the glycemic indexs and loads of the food and drink you regularly consume:
Practice Time Restricted Eating
TRE simply refers to eating (or not eating) within a predefined time window.
A ten hour restricted feeding period improves blood glucose and insulin sensitivity, results in weight loss, reduces the necessary dosage of hypoglycaemic drugs and enhances quality of life. It can also offer cardiovascular benefits by reducing atherosclerotic lipid levels [2].
There are many variant of TRE; for instance:
- 16:8 — 16 hours fasting, 8 hours eating. I do this regularly. I eat between noon and 7:00 PM, coffee, tea and water during the fasting hours. (See these posts on Intermittent Fasting.)
- 5:2 — 5 days eating normally, 2 days under-eating.
- Complete fasting for one or more days.
Exercise
Walk after meals, and do resistance training.
“People would be dumbfounded at how much a walk after meals lowers their glucose and their insulin“, says Dr. Bikman, “because the moment you start moving those muscles, they don’t need insulin to tell them what to do, they just start pulling in their own glucose. They get so greedy, so demanding, that they don’t have to wait for insulin to open those glucose doors, they open them on their own, driving down the blood glucose, which helps the insulin stay much than it would’ve been otherwise, so movement matters.”
Try to walk at a brisk pace.
By “resistance training“, I’m referring to calisthenics and weight lifting. Dynamic strength training improves insulin sensitivity in men with insulin resistance independently on weight loss or increase in aerobic capacity. Clearly, dynamic strength training is an appropriate physical activity for management of the insulin resistance [3]. And not for men only — same with women [4].
If you need some ideas about how to exercise against resistance, I’ve got you covered here.
Reduce Stress
Dr. Bikman says that his research shows stress hormones like epinephrine and cortisol “absolutely cause insulin resistance and tremendously matter”.
Chronic stress also elevates baseline inflammation, and high chronic inflammation is another cause of insulin resistance.
You can reduce your stress by:
- The 4x4x4 breath, and
- Meditation.
The 4x4x4 breath is a technique practices by the US military to stay calm when bullets are whizzing by. I described it at length here, but suffice to say, do this:
- Get in a relaxed position
- Inhale thru your nose for 4 seconds, expanding your chest, abdomen and back.
- Hold for 4 seconds.
- Exhale thru your nose for 4 seconds.
- Pause for 4 seconds.
- Repeat.
Keep doing this until whatever was stressing you has vanished.
Meditation can be a long-form of the 4x4x4 breath technique. There are many ways to meditate, and if that’s of interest, go knock yourself out with my posts on that topic.
Supplementation
Drs. Hyman and Bikman recommend the following supplements that can help reduce insulin resistance:
- Magnesium
- Alpha-lipoic acid
- Omega-3 fats,
- Vitamin D
- Cinnamon
- Berberine
- Amla
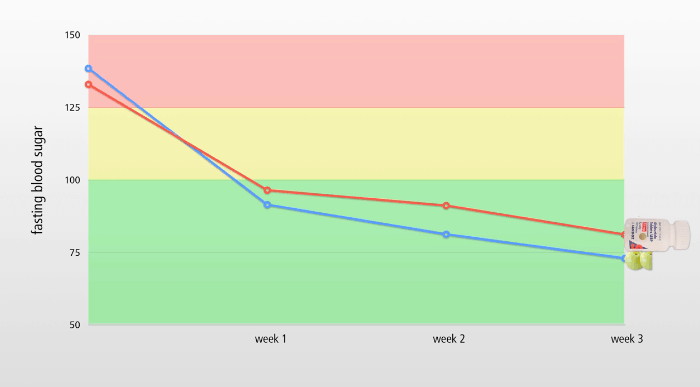
Those last two — berberine and amla — are a great one-two punch for reducing blood sugar. See my post, You Absolutely Need To Lower Your Blood Sugar, where I’ll explain this:
Your “Test Your Insulin Sensitivity” Takeaway
We covered a lot of ground in this post, so let’s keep this “takeaway” concise and simple.
Remember these four things:
- Only 1 in 8 Americans have optimal metabolic health, which means that most of us should test our insulin sensitivity, and get to work if we are insulin resistant.
- Insulin resistance causes several downstream health issues, such as metabolic syndrome, inflammation, body fat, the feminization of men and the masculinization of women.
- You can test your insulin sensitivity by various blood tests and by measuring your waist-to-height and waist-to-hips ratios.
- You can reduce insulin resistance by eating foods with a low glycemic load, exercising, reducing stress, and with supplements.
If you know people who could be helped by this post, send it to them!
Last Updated on February 7, 2024 by Joe Garma